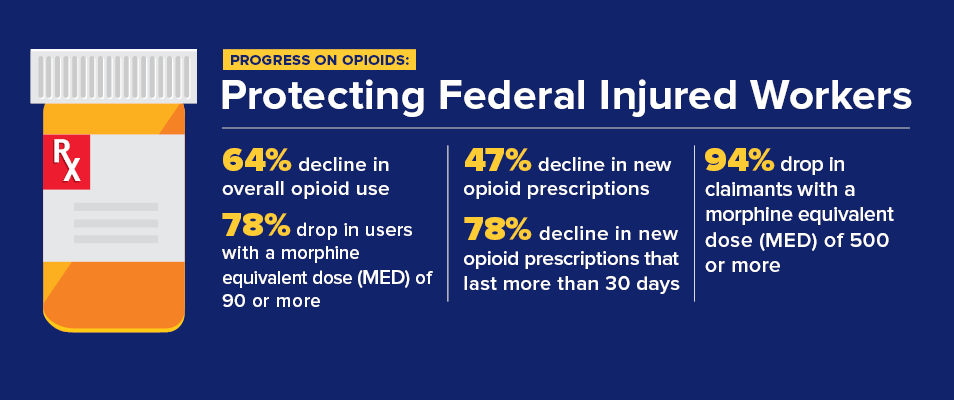
OWCP has implemented a four-point strategic plan to combat the opioid epidemic and reduce the potential for opioid misuse and addiction among injured federal workers.
 1. Effective Controls
1. Effective Controls
Approach: Institute broad general controls followed by targeted controls
 2. Tailored Treatment
2. Tailored Treatment
Approach: Apply a compassionate, individualized treatment approach to every injured federal worker receiving opioids
 3. Impactful Communications
3. Impactful Communications
Approach: Issue communications using both general and targeted messaging
 4. Aggressive Fraud Detection
4. Aggressive Fraud Detection
Approach: Eliminate fraud and abuse in the federal workers' compensation system
 Take Back Days
Take Back Days
"Make them describe before they prescribe"
Discuss the risks of opioid use and alternative forms of pain management with your physician before starting or refilling opioid prescriptions.
For more information on safely disposing of medications, including opioids, please visit the U.S. Food and Drug Administration (FDA) website.
To locate places near you to safely dispose of unwanted medications, including opioids, please visit the Drug Enforcement Agency (DEA) website.
Additional Resources
- OWCP's Approach to Combating Opioid Use and Misuse
- Opioid Alert for Newly Injured Workers
- Risk Factors for Opioid Misuse, Addiction, and Overdose
- Opioid Report: Patterns of Chronic Higher-Dose and Lower-Dose Opioid Use in Federal Workers' Compensation Claimants
- Centers for Disease Control and Prevention: Guideline for Prescribing Opioids for Chronic Pain
Opioid-Related Program Bulletins
- 19-04: New Opioid Prescribing Guidelines in the FECA Program Limiting Initial Fills to Seven Days and Imposing LMN at 28 Days
- 18-06: Alternative Pain Management and Treatment for Opioid Use Disorder
- 18-04: Prescribing Guidelines, Short-Term, Long-Term and High Dose Opioid Use
Need Help? If you or someone you know needs help dealing with opioid abuse please visit FindTreatment.gov or call 1-800-662-HELP (4357)
