Division of Federal Employees' Compensation (DFEC)
FECA Part 3
|
Chapter |
Subject |
|---|---|
|
Paragraph and Subject |
Date |
Trans. No. |
|---|---|---|
|
Table of Contents |
09/95 |
95-39 |
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
04/93 |
93-24 |
|
|
09/95 |
95-39 |
1. Purpose. This part of the procedure manual describes for both physicians and claims personnel the procedures for administering the medical care program under the Federal Employees' Compensation Act (FECA). Examination of case files and authorization of medical care are conducted through the cooperative efforts of the Medical Unit and the Claims Units within each district office.
Back to Chapter 3-0100 Table of Contents
2. Benefits. The FECA provides the following benefits for Federal employees:
a. Medical Care. Services prescribed or recommended by a qualified physician which are likely to cure, give relief, reduce the degree or the period of disability, or aid in lessening the amount of monthly compensation may be authorized. These services include surgery and hospitalization as well as appliances and supplies.
b. Disability Benefits. Compensation is paid for lost wages resulting from the employment-related injury, disease or illness.
(1) Total Disability. A claimant is paid compensation for total disability when the employee is medically unable to perform gainful employment due to employment-related injury, disease or illness. The loss of use of both hands, both arms, both feet or both legs, or the loss of sight of both eyes, is considered prima facie evidence of permanent total disability (section 8105 (b) of FECA), though claimants with these disabilities are sometimes still able to work.
(2) Partial Disability. Reduced benefits are paid when the employee is not totally disabled but is capable of performing duties which are compatible with the medically imposed work limitations resulting from the injury, disease, or illness. The amount of compensation paid commensurate with the employee's loss of wage-earning capacity (sections 8106 and 8115 of FECA).
c. Schedule Award. Compensation for permanent impairment of certain members or functions of the body may be paid regardless of the employee's ability to work. A schedule award is payable when the condition has reached maximum medical improvement. The AMA Guides to the Evaluation of Permanent Impairment form the basis for awards. Awards are also payable for disfigurement of the face, head or neck which is likely to handicap the claimant in maintaining or securing employment (section 8107 of the FECA).
d. Vocational Rehabilitation. Vocational rehabilitation services are provided when an injured employee is unable to return to his previous work (section 8104 of FECA).
e. Death Benefits. A range of benefits for the dependents of an employee whose death was employment-related is provided (sections 8133 and 8134 of the FECA).
f. Miscellaneous Benefits. Other benefits include reimbursement for transportation costs incurred in obtaining medical treatment or rehabilitation services. Nursing and other paramedical services are included when they are likely to be beneficial, and an attendant's allowance is payable in addition to compensation to severely disabled claimants.
Back to Chapter 3-0100 Table of Contents
3. Definitions. By statute, the term "physician" includes surgeons, podiatrists, dentists, clinical psychologists, optometrists, osteopathic practitioners, and chiropractors within the scope of their practice as defined by state law.
a. Psychologists. OWCP has accepted the American Psychological Association's definition of a clinical psychologist as an individual who:
(1) Is licensed or certified as a psychologist at the independent practice level of psychology by the state in which he or she practices, and
(2) Either possesses a doctoral degree in psychology from an educational institution accredited by an organization recognized by the Council on Post-Secondary Accreditation or is listed in a national register of health service providers in psychology which the Secretary of the Department of Labor deems appropriate, and
(3) Possesses two years of supervised experience in health service, at least one year of which is post degree.
b. Chiropractors. These practitioners are defined as "physicians" only to the extent that their reimbursable services are limited to treatment consisting of manual manipulation of the spine to correct a subluxation as demonstrated by X-ray to exist. A chiropractor has the right to interpret his or her own X-rays to determine whether they support the diagnosis of subluxation and to determine any period of disability resulting from that condition. OWCP defines subluxation as an incomplete dislocation, off-centering, misalignment, fixation or abnormal spacing of the vertebrae.
c. Physicians' Assistants. These practitioners, who are not physicians under the Act, receive academic training and clinical experience and may be certified by the National Commission on the Certification of Physician's Assistants. A report prepared by a physician's assistant which is countersigned by a physician should be accepted as medical evidence.
d. Religious Practitioners. The Christian Science Church permits treatment of its members only by its own practitioners, though it has no objection to periodic examinations to determine entitlement to compensation and to assess whether maximum medical improvement has been reached. The FECA does not authorize treatment by nonmedical practitioners of the healing arts, such as psychic healers or faith healers, although they may be permitted at the claimant's expense.
Back to Chapter 3-0100 Table of Contents
4. Subjects Covered. The roles of the District Medical Director, District Medical Adviser, Medical Management Assistant, and Staff Nurse are discussed briefly in Chapter 3-200, and the Staff Nurse's work is addressed more fully in Chapter 3-201. Chapter 3-202 addresses certification procedures for contract nurses. The procedures for authorizing treatment and the provision of supplies are described in Chapter 3-300, while treatments and supplies which may be authorized under the FECA are detailed in Chapter 3-400. The process of obtaining medical evaluations is described in Chapter 3-500, and requirements for medical reports are detailed in Chapter 3-600. Schedule award determinations are considered in Chapter 3-700. Procedures for excluding a medical provider are detailed in Chapter 3-800, and administrative matters are considered in Chapter 3-900.
Back to Chapter 3-0100 Table of Contents
|
Paragraph and Subject |
Date |
Trans. No. |
|---|---|---|
|
Table of Contents |
05/94 |
94-24 |
|
04/93 |
93-24 |
|
|
04/93 |
93-24 |
|
|
04/93 |
93-24 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
|
04/93 |
93-24 |
|
04/93 |
93-24 |
1. Purpose. This chapter describes the roles and responsibilities of OWCP medical staff, which usually includes a senior Federally employed physician as District Medical Director, (DMD), one or more District Medical Advisers (DMA), one or more Medical Management Assistant(s) (MMA), and a Staff Nurse.
Back to Chapter 3-0200 Table of Contents
2. Structure of the Medical Unit. The responsibility for oversight of the Office's medical benefits program is vested in the DMD, who works under the medical guidance of the OWCP National Office Medical Director and the administrative supervision of the Regional Director (RD) or the District Director (DD). A district office may have one or more DMAs (usually contract employees), and the functions of each office's Medical Unit are aided by one or more MMAs. The Staff Nurse coordinates the work of the Field Nurses who act on behalf of each district office in the case management process.
Back to Chapter 3-0200 Table of Contents
3. District Medical Director (DMD). The functions of the DMD include the following:
a. Establishes liaison with regional professional societies State health departments, and individual providers within the district office's jurisdiction. The DMD can familiarize the medical community with the nature of the program and its needs and objectives. Specific areas which may be addressed include types of medical reports and their use within the program; requirements for content and quality of medical reports and the impact of these factors on the length of the adjudicatory process as well as continued use of a particular consultant; the Office's commitment to the rehabilitation of the employee and the resources available to this end; and new policies and procedures as warranted.
Such meetings allow the DMD to transmit concerns and suggestions from the medical community to district office managers. These contacts may be arranged by the DMD alone, or by the DMD in conjunction with district office management, and it may take the form of contacts with local medical societies and other groups of physicians such as the medical staff of local hospitals, and providers in group practices. The DMD may also obtain from district office files the names of physicians who have served as consultants in cases involving a particular disease, such as asbestosis, and sponsor meetings to discuss changes in diagnosis and treatment as well as administrative matters.
b. Visits with major employing agencies within the district office's jurisdiction. The DMD can also perform a useful function by encouraging employing agency personnel to conduct limited outreach efforts with physicians in their respective geographic areas. Such efforts may include tours of the employing agency and demonstrations of the types of light duty which may be available to partially disabled workers, so that physicians will be more aware of options other than continuing the claimant on total disability.
c. Identifies and evaluates the credentials of physicians willing to serve as consultants (DMAs) to manage workloads. (The method of selecting a consultant for this function is identical to the procedure for obtaining second opinion examinations, which is described in Chapter 3-900).
d. Establishes and administers a network of medical specialists (second opinion specialists) and DMAs who provide the Office with medical opinions (see Chapter 3-900).
e. Provides training and guidance to Claims Examiners (CEs) and other district office staff regarding medical issues. The DMD may properly advise CEs concerning the tone and content of letters sent to members of the medical community. He or she may provide formal and/or informal training on common conditions and medical treatment issues to the district office staff. The DMD also has an advisory role to bill pay staff within the district office.
f. Identifies and reports medical trends to district office management and the OWCP Medical Director. The DMD advises the DD or RD concerning customary ranges of fees for various services in the area and advises the RD concerning exclusion of medical providers. The DMD will monitor the performance of referral specialists and advise the DD or RD of physicians whose reports are consistently incomplete, unreliable, or late.
g. Provides professional opinions and technical advice in connection with the adjudication and management of complex claims.
The DMD does not perform medical examinations or functions of a clinical nature except for participating in evaluation of claimants who seek an award for disfigurement of the face, head or neck (see Chapter 3-700). Moreover, while the DMD does not act in a supervisory capacity per se, he or she does have administrative oversight with respect to the medical functions of the district office.
Back to Chapter 3-0200 Table of Contents
4. District Medical Adviser (DMA). The functions of the DMA (and the DMD insofar as he or she performs medical evaluations of case files) include interpretation of medical reports; rendering medical evaluations in his or her own right; and providing guidance or instruction to claims staff regarding general medical issues which are in compensation claims.
a. Interpreting Medical Reports. The CE seeks the interpretive function of the DMA where the medical evidence is complete and sufficient prior to such review. In this form of review, the DMA may determine the percentage of permanent partial impairment, evaluate test results, or "translate" technical language. The DMA may also be asked to review reports from referee specialists where a schedule award is at issue (see Chapter 3-600).
b. Rendering Medical Evaluations. The CE seeks advice from the DMA to proceed with developing and weighing the medical evidence where the report from the attending physician, second opinion or referee specialist is not clear and well rationalized, and the DMA provides written opinions on medical questions posed by members of the claims staff.
In this capacity, the DMA may advise whether a claimant's condition is employment-related, whether the effects of an accepted condition continue, and whether the claimant is receiving appropriate medical care, including whether recommended procedures, appliances or treatment are useful or necessary. The DMA may also be asked to comment on proper development of the medical evidence where an unusual condition is under consideration.
The Employees' Compensation Appeals Board has addressed the role of the DMA in its decision in the case of Carlton L. Owens, 36 ECAB 608:
The role of the Office medical adviser is to act as a consultant in reviewing cases under the Federal Employees' Compensation Act. Claims examiners make use of the services of medical advisers in adjudicating the issues of causal relationship, extent of disability, degree of permanent impairment, and suitability of work. The Office medical adviser's role is not to act in an adjudicatory capacity or address legal issues in the case, and the Office should carefully observe the distinction between adjudicatory questions which are not appropriate and medical questions which are appropriate.
c. Monitoring Medical Care. While the DMA does not routinely monitor cases to ensure adequacy of medical care, he or she is expected to recognize issues regarding the quality of care arising in the cases he or she evaluates. CEs may also identify cases where the propriety of medical care is in question and should refer them to the DMA for action or advice. Issues may include:
(1) Appropriateness/Usefulness of Treatment. The criteria used in assessing the suitability of medical care as well as Office policies regarding specific treatments and appliances which may be authorized are discussed in Chapter 3-400.
(2) Length of Treatment. The duration or frequency of treatment appears excessive for the condition or incompatible with the norm for the medical community.
(3) Transfer of Medical Care. Claimants not infrequently request changes in attending physician, but the Office seldom initiates this action. Transfers of care should be handled according to the claimant's medical needs with due regard for medical protocol.
A case sent to the DMA for evaluation of another matter may reveal issues pertaining to the suitability of medical care, and the DMA is expected to use his or her medical expertise to recognize such problems and bring them to the CE's attention.
Back to Chapter 3-0200 Table of Contents
5. Medical Management Assistant (MMA). The MMA's function is to assist the DMD in the administration of the Medical Unit and to perform associated support functions, which include:
a. Screening. The MMA examines incoming case files to ensure that all necessary information is present, including a list of questions and Statement of Accepted Facts.
b. Scheduling. The MMA schedules appointments for second opinion and referee examinations in accordance with the Office's procurement and rotation policies and the specific requirements of each type of examination.
c. Advising of Arrangements. The MMA prepares letters to claimants and physicians once such examinations have been scheduled and ensure that all necessary information and material is provided to each party.
d. Record-Keeping. The MMA maintains records concerning utilization of physicians in each category as well as logs pertaining to prompt payment of bills; keep records of cases out of the office and contact physicians when reports and cases are overdue.
e. Documenting Exclusion Data. The MMA maintains information concerning exclusion of medical providers and ensures that documentation of alleged infractions is routed to the correct parties within the district office.
f. Keying. The MMA may key outgoing cases to other parts of the district office. The MMA ensures that location printouts reflect only the cases actually present in the medical unit, and initiates searches for any other cases.
Back to Chapter 3-0200 Table of Contents
6. Staff Nurse. The OWCP Staff Nurse is responsible for coordinating the nurse intervention process in the district office, which in turn is directed toward managing disability claims to facilitate recovery and, if possible, return to work. This function includes:
a. Selecting cases for intervention, in some district offices, and assigning them to Field Nurses with the CEs' concurrence.
b. Acting as liaison between the Field Nurses and CEs. This function includes answering questions from both parties, interpreting OWCP practices to the Field Nurses, and helping the CEs to understand the nurses' role in managing cases.
c. Procuring and selecting enough field Nurses to provide high quality services to OWCP claimants, and managing and monitoring their activities on a case by case basis as well as cumulatively.
d. Training Field Nurses on intervention procedures and formal and informal training of CEs and OWCP staff on these procedures and other medical topics as warranted in the particular office.
e. Performing other liaison activities such as outreach to the medical community and scheduling certain second opinion and impartial examinations to ensure that these are performed in a timely fashion and the resulting reports address CEs' concerns fully.
See PM 3-201 for a fuller discussion of the Staff Nurse's duties.
Back to Chapter 3-0200 Table of Contents
|
Paragraph and Subject |
Date |
Trans. No. |
|---|---|---|
|
Table of Contents |
11/98 |
99-06 |
|
04/93 |
93-29 |
|
|
04/93 |
93-29 |
|
|
04/93 |
93-29 |
|
|
04/93 |
93-29 |
|
|
04/93 |
93-29 |
|
|
04/93 |
93-29 |
|
|
09/95 |
95-39 |
|
|
04/93 |
93-29 |
|
|
08/94 |
94-34 |
|
|
10/95 |
96-04 |
|
|
09/96 |
96-15 |
|
|
09/96 |
96-15 |
|
|
09/96 |
96-15 |
|
|
09/96 |
96-15 |
|
|
09/96 |
96-15 |
|
|
09/96 |
96-15 |
|
|
09/96 |
96-15 |
|
|
09/96 |
96-15 |
|
|
11/98 |
99-06 |
|
Exhibits |
Date |
Trans. No. |
|---|---|---|
|
12/94 |
95-04 |
|
|
12/94 |
95-04 |
|
|
12/94 |
95-04 |
|
|
12/94 |
95-04 |
|
|
12/94 |
95-04 |
|
|
12/94 |
95-04 |
|
|
12/94 |
95-04 |
1. Purpose and Scope. The role of the Staff Nurse in the FEC district offices is to aid in managing disability cases. The Staff Nurse's role and functions in this process are the subject of this chapter. Included in the discussion will be specific nursing functions, intervention and liaison activities which will assist the Claims Examiner (CE) in managing cases.
Back to Chapter 3-0201 Table of Contents
2. Definition. In its broadest scope, case management is a comprehensive approach to minimize the length and perhaps the extent of disability in some compensation cases. In this process, nurses will play a vital role by participating in the early, aggressive medical management of cases. The primary focus of the nurses' activities will be to encourage recovery and the return to work through direct interventions with the claimants, treating physicians, and employing agencies.
Back to Chapter 3-0201 Table of Contents
3. Nurses' Roles in the District Offices. Nurses involved in case management may be OWCP staff members or private sector professionals working with the program on a contractual basis. While the latter (Field Nurse) can perform only the actual interventions, the OWCP Staff Nurse may coordinate nurse intervention as well as actually intervening in cases.
a. The Nurse Intervenor Role. The Staff or Field Nurse functioning in this role will be working closely with OWCP office staff and claimants, physicians in the community, and employing agencies to assist in the return to work effort. For clarity, a nurse acting in this role will be designated as Field Nurse throughout this chapter.
b. The Nurse Coordinator Role. The OWCP Staff Nurse acting in this capacity is responsible for coordinating the nurse intervention process in the district office. This function includes:
(1) Selecting cases and assigning them to the Field Nurse(s),
(2) Managing Field Nurses and monitoring their activities on a case by case basis as well as cumulatively,
(3) Acting as liaison between the Field Nurses and CEs,
(4) Procuring and selecting enough field Nurses to provide high quality services to OWCP claimants,
(5) Training Field Nurses on intervention procedures and formal and informal training of CEs and OWCP staff on these procedures and other medical topics as warranted in the particular office, and
(6) Performing other liaison activities such as outreach to the medical community and scheduling certain second opinion and impartial examinations to ensure that these are performed in a timely fashion and the resulting reports address CEs' concerns fully.
Back to Chapter 3-0201 Table of Contents
4. Types of Nurse Intervention. The nurse intervention process can be classified according to the degree of interaction: limited, moderate or intensive. The Staff Nurse determines the appropriate type of intervention based on the diagnosis, the severity of the injury or illness and demographic considerations.
a. Limited intervention consists of telephone interaction only. This method provides the ability to reach a greater number of claimants and is most effective in uncomplicated sprains and strains with a delayed return to work date. Phone contact is initiated with the claimant and details of the injury are discussed. In the follow-up phone calls, the nurse reinforces the treatment regimes of the treating physician and formulates return to work plans with the claimant and treating physician.
While phone contacts are not restricted as to frequency, the nurse must keep in mind that too many phone contacts may inadvertently reinforce patients who exhibit high levels of pain and illness behavior. If contacts are set up on an as-needed basis, patients having the most difficulty will likely get the most contact. Intervention, to be effective, should be completed within four months.
b. Moderate intervention combines both phone calls and face-to-face interaction. This type of intervention begins with phone contact but as the intervention continues, evolving circumstances may warrant face to face contact.
For example, if in the course of phone intervention, it becomes apparent that the claimant's physician is planning surgery, a re-operative/post-operative visit by the nurse will assist to reinforce return to work goals. Typically, these interventions will not exceed four months' duration. However, there will be cases (complicated post-operative period) requiring an extension of the nurse's time, and the CE must provide authorization for this extension.
c. Intensive intervention is reserved for catastrophic cases such as head or spinal cord injuries with extensive functional deficits where the medical recovery is expected to extend over long or indefinite periods of time. In these cases, the immediate intervention is directed at the claimant's needs during the acute phase of injury (coordinating hospital care with the variety of specialists in the case) and continues until stabilization (e.g., placement in a rehabilitation facility or home with modifications) has been achieved and vocational rehabilitation can be recommended.
Usually vocational rehabilitation services do not begin until nurse services end, but in these cases it may be important to begin vocational counseling during the period of nurse intervention. The Field Nurse assigned to the case is responsible for identifying cases that may benefit from vocational services. He or she should communicate this recommendation to the CE involved in the case.
Back to Chapter 3-0201 Table of Contents
5. Phases in the Intervention Process. The intervention process, regardless of the type, can be divided into four stages as briefly described below. Throughout each phase, the nurse monitors the quality of medical care rendered to the claimant and communicates frequently with the CE regarding the claimant's progress.
a. Identification Phase. The Staff Nurse, CE or other staff identifies cases for intervention according to standard criteria. Communication is initiated with all parties: claimants, treating physicians and employing agencies.
b. Monitoring Phase. The Field Nurse reviews the physician's overall treatment plan and identifies areas needing CE attention (prior authorization for surgery, prolonged bed rest, etc.) As necessary, the nurse discusses issues with the parties concerned and participates in updating or modifying the treatment plan to fit the claimant's changing health status.
c. Assessment Phase. The Field Nurse determines whether return to work is possible and whether return to work plans are available and feasible. Collaborates with all parties (CE, physician, agency, claimant) to implement the return to work.
d. Discharge Planning Phase. The Staff Nurse assesses the outcome of the intervention and, as necessary, follows up in the case to ensure continuity in its management. If the claimant has returned to work, the Field Nurse will provide follow-up for 60 days. In cases where the nurse intervention period has expired and the return to work has not occurred, the Staff Nurse will refer the case to the CE with appropriate recommendations such as referral for vocational rehabilitation services, second opinion, etc.
Back to Chapter 3-0201 Table of Contents
6. Preliminary Steps. Nurse intervention early during the period of disability is one of the major components of the quality case management procedures. This section details all the important aspects and steps in this process.
a. Criteria for Case Selection. Cases which have been traditionally associated with poor outcomes in terms of return to work, cases where the outcome is uncertain, and cases where specific medical issues need to be clarified, should be referred for nurse intervention.
(1) Traumatic Injury Cases. Although the ideal time for nurse intervention is from 45-90 days after the day of injury, the CE may refer traumatic injury cases for nurse intervention regardless of the time elapsed since the injury if:
(a) The medical evidence does not state a return to work date;
(b) The return to work date is unrealistic (i.e., not in keeping with the magnitude of the original injury);
(c) The return to work date is extended without clear medical reasons;
(d) The claimant is partially disabled but the file does not contain a description of work limitations;
(e) The CE requires additional medical information for the initial or continuing authorization of unusual and/or prolonged services such as intensive home nursing, housing modifications and extensive surgery or physical therapy.
(2) Occupational Illness Cases. These cases ordinarily require more than 90 days to adjudicate, thus placing them outside the optimum time frame for nurse intervention. Therefore they will not routinely be referred for continuing nurse intervention, though they may be referred for advice and assistance with particular issues [see paragraph a(1)(e) above]. Referral for vocational rehabilitation services will likely be more appropriate in most occupational illness cases.
b. Sources of Cases for Nurse Intervention.
(1) CE Referrals. CEs are tasked with identifying cases that meet the criteria indicated above. The CEs will identify a significant number of these cases at the time of the authorization for the first compensation payment (excluding most leave buy-backs and schedule awards).
(2) Automated Reports. Staff Nurses may identify cases that meet the above criteria using automated reports of CA-7 payments or other reports containing similar information.
(3) Other Sources. In some instances, employing agencies, Vocational Rehabilitation Specialists, District Medical Directors or Advisors and others can identify cases which may benefit from nurse services. All cases referred in this fashion should be discussed with the CE before nurse intervention is offered to the claimant since the final authority to intervene with the claimant remains a prerogative of the CE.
c. Work/No Work Call. The initial interaction with claimants occurs during the initial telephone call. The purpose of this call is to ascertain the work status of the claimant and to inform those claimants who meet the above indicated criteria of the intended nurse intervention in his or her case. The CE may make this call. However, in those offices where the Staff Nurse identifies potentially eligible cases from automated reports, this call will be the responsibility of the OWCP Staff Nurse and he or she should follow the steps detailed below:
(1) If the claimant has returned to full duty, the nurse notifies the CE. In most instances, the nurse recommends that further intervention is not necessary. However, in some cases where the nurse has reason to believe that the medical condition is unstable or that the claimant might stop working for other reasons, he or she may recommend a follow-up call in four weeks to verify that the claimant remains at work;
(2) If the claimant has returned to modified and/or part time duty, the nurse will notify the CE, who will make a decision as to whether the claimant is to be followed until he or she returns to full-time employment.
(3) If the claimant has not returned to work but knows when the return to duty will occur, and the date appears realistic according to the medical evidence, medical matrix or MEDGUIDE in Folioviews, the Staff Nurse sets up a call-up for the date specified and calls the employing agency on that date to find out if the claimant has in fact returned to work.
(4) If the claimant has not returned to work at the time of the follow-up call, and either does not state a plan to return to duty or offers a date inconsistent with the nature and severity of the injury, the nurse explains the nurse intervention program to the claimant and attempts to engage the claimant in the program.
(5) Once the call is completed, the nurse notifies the CE of the result using a Form CA-110 and recommending appropriate action on Form OWCP-57. Although the intervention program is voluntary, participation should be strongly encouraged. A claimant who refuses to be visited may nonetheless allow intervention by telephone. If the claimant refuses to participate altogether, the nurse ends the telephone conversation but reports this result to the CE. The nurse should attempt to secure a medical release from the claimant so that communication may be initiated with the attending physician.
Back to Chapter 3-0201 Table of Contents
7. Performing Interventions. The Staff Nurse selects the type of intervention needed based on the nature and severity of the claimant's condition, the claimant's geographic location and other factors. At the same time, he or she assigns the case to a nurse who will actually perform the intervention, and notifies the claimant, physician, employing agency and the CE.
a. Initial Contacts.
(1) Claimant. The Field Nurse notifies the claimant that they will be working together through the recovery stage. He or she also advises the claimant that the treating physician will be made a part of this collaborative return to work effort.
(2) Treating Physician. The Field Nurse will contact the treating physician to discuss current and future treatment regimes. Emphasis is placed on identifying and managing open-ended treatments such as bed rest and physical therapy, as well as prolonged therapy with pain medications. As necessary, the nurse may discuss medical issues with the District Medical Director (DMD) or Advisor (DMA), or may recommend a second opinion to clarify issues. Ultimately, a return to work date and concrete work limitations, if needed, will be discussed and formulated using Form OWCP-5. As with the claimant, contact is made initially by phone followed by a confirmation letter.
(3) Employing Agency. The agency will also be contacted by the Field Nurse. Communication with the agency begins with the claimant's supervisor or the injury compensation specialist because this person can furnish important information regarding the job in question as well as provide some sense of pre-existing interpersonal issues which may affect the return to work effort.
There are a variety of reasons for the nurse to contact the employing agency. For example, the nurse notifies the compensation specialist that one of their employees has been contacted by a nurse, verifies that the employee has or has not returned to work and, when applicable, informs the agency that the physician has imposed some physical limitations for the return to work.
b. Intervention Guidelines. The Field Nurse assigned to the case performs the intervention. The nurse is responsible for structuring the intervention in terms of the number, content and the length of contacts with the claimant and other parties involved. To do so, the nurse should keep in mind the following guidelines:
(1) The focus of the program is the return to work and the claimant should be encouraged to participate actively in the treatment plan and in the resolution of problems which may impact on the recovery effort.
(2) Visits or calls to the claimant should be scheduled on time-contingent basis rather than as a response to the appearance or exacerbation of symptoms.
(3) The treating physician should participate in this process by producing a treatment plan and a projected length of disability which are commensurate with the claimant's signs and symptoms. If these are not forthcoming or if the physician refuses to communicate with the nurse, the intervention with the claimant and employing agency should continue and the MD's refusal to participate should be communicated to the CE.
(4) Although the Field Nurse is responsible for structuring the number, length, content and medium (telephone, face-to-face) of the interactions with all participants, he or she should be aware that the intervention is a finite process. The intervention is limited to 120 days from the date of referral. In some instances, where there is substantive evidence that the return to work will occur shortly, the CE may authorize an additional period of 30 days. Once the period for nurse intervention has been exhausted, the case is referred to the CE for further action.
c. Intervention Process.
(1) During the first 30 days of intervention, the Field Nurse determines whether the physician has formulated a treatment plan and whether the claimant's physical condition is improving. As necessary, the nurse discusses the formulation or modification of the plan with the physician and the claimant.
As soon as the Field Nurse completes the visits with the claimant and treating physician, the nurse discusses findings from the visits and the subsequent plans for follow up action with the CE and the Staff Nurse. The DMD/DMA may be consulted to ensure that the treatment is appropriate for the claimant's condition. The CE is made aware of the need to authorize particular therapies, and that the return to work is part of the treatment plan.
Once the plan has been formulated, the nurse monitors the physical progress of the claimant and obtains a return to work date from the physician, when appropriate. If necessary, the nurse forwards a OWCP-5 form to the treating physician to define the work restrictions present and the level of function of the individual. He or she may discuss the content and the use of the form by OWCP and the employing agency with the physician.
The nurse may also recommend a second opinion examination, and with the CE's concurrence, schedule it. However, if the physician selected is not listed in the Physicians' Directory System, the nurse should advise the Medical Management Assistant of the physician's name and address so that this information can be added to the system.
(2) The nurse works with the employing agency to ensure that the physical demands of the job are in keeping with any restrictions imposed by the physician, that there are no significant barriers to the return to work, and verifies that the return to work occurs on or near the expected date.
If the return to work is delayed, the Field Nurse communicates this to the CE and discusses the reasons with all parties concerned as necessary. The nurse endeavors to re-establish the return to work emphasis, define a new date and verify that indeed the claimant returns to work on or near the expected date.
(3) If the return to work date obtained is not within 120 days from the beginning of the intervention, there is no significant improvement in the condition of the claimant, or the physician does not produce a plan, the Staff Nurse ends the intervention and refers the case to the CE for action. Upon closing the case, the Staff or Field Nurse may choose to offer specific recommendations such as referral for a second opinion examination, referral to vocational rehabilitation, or change of physician.
(4) If the claimant does not return to work on or near the return to work date, or remains at work less than 60 days, the nurse needs to determine the underlying reasons and take appropriate action. If a job adjustment problem (difficulty with the employing agency) is the cause for the continuing lack of employment or stopping work, the nurse refers the case to the CE for further action, clearly stating the nature of the problem.
However, if medical problems prevent or cut short the return to work, the nurse ensures the completion of OWCP-5 by the physician, closes the intervention and refers the case to the CE. Where the OWCP-5 indicates that the claimant is able, or will be able, to work four hours or more, the nurse recommends vocational rehabilitation services. The SN may complete Form OWCP-14 to refer the case for vocational rehabilitation services, but may not sign the form. The actual referral remains the CE's responsibility.
If there are no job adjustment or medical problems, but the nurse has reason to believe that there is non-cooperation on the part of the claimant, he or she refers the case to CE for further action, presenting well reasoned justification for his or her opinion.
(5) The CE may decide that a conference call involving the injured worker, employing agency, Field Nurse, Staff Nurse, CE and Senior CE will help clarify return to work issues at this point.
d. Case Closure. Nurse intervention can result in various outcomes. If the intervention has been continuing in nature, the expected result is the return to work. In most instances, the claimant will return to the pre-injury position, with or without modifications, or to a light duty arrangement. Although it is possible that the worker will return to a position outside of his or her agency during the nurse intervention period, this is not considered likely. In a number of cases, the return to work will not occur within the intervention time frames. In both instances, the Staff Nurse will ultimately close the case from the nurse intervention viewpoint and refer it to the CE for further action.
(1) To ensure that the adjustment to work is satisfactory, contact is made with the claimant at least three times during the course of 60 days: on the first day of work, at the end of the first month and at the end of the 60 days. The Field Nurse will accompany the claimant to the facility on the first day back on the job. A meeting is held by the Field Nurse with all concerned (claimant, supervisor, injury compensation specialist) to confirm an understanding of the basis of the return to work requirements and to clarify roles.
Should the Field Nurse identify physical or psychological barriers, deterioration of the medical condition, or any other indication that the return to work may not be successful, he or she contacts all interested parties as necessary to resolve the issues within the 60 day time frame. Monitoring the return to work beyond this period requires CE approval.
(2) At the end of the 60 days or later if an additional follow-up period has been approved, the Field Nurse prepares a memorandum to the Staff Nurse describing the intervention, the type of work accepted by the claimant, and the date of the placement. In turn, the Staff Nurse forwards the memorandum to the CE assigned to the case, closes the case from a nursing viewpoint and notes the return to work in the tracking system.
(3) If the claimant does not return to work during the intervention, does not remain at work for 60 days, or does not accept the intervention or cooperate with the nurse, the Field Nurse prepares a memorandum for the Staff Nurse stating the problem and recommending closure of the case and a future course of action (second opinion, change of physician, referral to vocational rehabilitation, etc.) The Staff Nurse reviews the case and the Field Nurse reports, closes the case if warranted and advises the CE of the particular issues of the case and makes appropriate recommendations.
Back to Chapter 3-0201 Table of Contents
8. Extensions and Interruptions of Nurse Services. The nurse intervention will usually last 120 days or less. In catastrophic injury cases, or in cases where the time and/or dollar limits are exceeded by small amounts and it is clear that the claimant will return to work within a short period of time, the intervention may extend beyond this limit if the CE authorizes extensions of time or money.
Extensions of services may also be necessary or desirable in other cases to ensure that initial return to work is successful, or to help the claimant reach higher levels of physical capacity, resulting if possible in return to full-time full duty. Extensions may also be granted if work-related surgery is necessary, or if the injury is a catastrophic one. Interruptions of services may be desirable because other medical conditions, either work-related or not, hinder the return to work effort.
a. Extensions.
(1) Initial Return to Work. The CE may approve a 30-day extension (60 days if requested so that the nurse can provide follow-up services after return to work). During this period, the Field Nurse may charge for 60 professional hours or $3,000, whichever comes first.
(2) Increase in Duty Status. Where the claimant has not returned to full-time full duty, the FN should stress the need to return to maximum functioning and work potential. The FN should also continue to pursue increases in work tolerance limitations and obtain descriptions of them on Form OWCP-5 at periodic intervals if the claimant does not return to full-time full duty. These attempts should be made at approximately two to three week intervals unless the facts of the case suggest a different plan.
After the 60-day follow-up period ends, the FN may continue to work toward full-time full duty if the medical evidence shows that such an outcome is likely. The FN and the Staff Nurse should recommend additional time in increments of no more than 30 days each, up to a total of 60 days. The CE must authorize each increment.
(3) Need for Surgery. Below are listed some common surgical procedures and their usual recovery times. In general, the simple procedures should require no more than 8-10 hours of professional services within the 30-day period. The moderately complex procedures will require about 12-16 hours of services within the 60-day period. Since the complex procedures will typically result in work limitations which may warrant referral for vocational rehabilitation services, the FN should work toward stabilizing the claimant's condition and obtaining Form OWCP-5 in these cases.
|
TYPE OF SURGERY
|
PROCEDURE
|
EXTENSION
|
|---|---|---|
|
A. Simple,
|
Endoscopies,
|
30 day extension,
|
|
B. Moderately
|
Discectomies
|
60 day extension,
|
|
C. Very complex
|
Multiple
|
Work with claimant
|
b. Interruptions. Return to work may be affected by other medical conditions (work-related or not), including pregnancy. The CE must approve interrupted status, which should not continue more than six months. The status code "NIN" (Nurse Interrupt) should be used.
(1) Concurrent Conditions. For a concurrent non-work-related condition, or surgery (whether work-related or not), the SN should determine whether continued FN services will likely be needed within six months. If so, and the CE concurs, the SN should place the case in interrupted status until the time of expected recovery. (Interrupted status, rather than an extension, is appropriate since the claimant would require little or no active involvement by the FN during this time.)
(2) FN Actions. During the interruption, the FN should stay in touch with the claimant to monitor medical issues and maintain a focus on return to work. If surgery is involved, the FN will typically review the attending physician's orders with the claimant after surgery and monitor the claimant's course at home. Also, the FN may discuss the post-operative plan with the physician by telephone and monitor the claimant's compliance with these orders. The RN may perform these services up to five hours per month.
Back to Chapter 3-0201 Table of Contents
9. Communications between the CE and the RN. The Field Nurse should inform the Staff Nurse of the medical progress of the claimant and of issues which may hinder the recovery process. As necessary, the nurse should provide thoughtful recommendations for further action. An initial evaluation after the first contact with the claimant and the treating physician, and monthly reports thereafter are expected. For these reports, the nurse uses the Initial Evaluation and Progress Report Form shown in Exhibits 1 and 2.
Periodically during the intervention and/or at the end of 120 days, the nurse and the CE or Staff Nurse will confer, either by mail, written memorandum or face-to-face meeting, to determine the next actions to be taken. The nurse is encouraged to communicate either with the CE or the Staff Nurse informally as well as by written report whenever this is necessary during the return to work effort.
Back to Chapter 3-0201 Table of Contents
10. Tracking the Nurse Intervention. Using the data described below, the Staff Nurse will be able to analyze various aspects of the program and obtain the basic statistics necessary to manage the nurse intervention effort. These statistics include: the numbers of claimants and nurses participating in the intervention program at any given time, the duration and result of the intervention by case or in a cumulative fashion in the district office, the rotation of cases among the Field Nurses and other data.
a. Claimant Data. From the moment a claimant is selected for intervention, the Staff Nurse or another designated individual must track the case through the Case Management File (CMF) Tracking System and, in district offices where it is installed, the Nurse Tracking System (NTS). The CMF system will include the dates on which the case is referred from the CE to the Staff Nurse and then to the Field Nurse. A return to work date is also captured on this system.
b. Field Nurse Data. Information regarding the Field Nurses should also be maintained, including the name of each nurse, his or her geographic location, and hourly rate.
Back to Chapter 3-0201 Table of Contents
11. Liaison Activities. By definition, case management includes the referral of certain injured workers for second opinion and referee examinations by medical specialists to ensure the appropriateness of the treatment plan, verify the level of disability and address other issues related to the medical recovery. To have the expected impact, these examinations need to occur on a timely basis.
At district office option, the Staff Nurse can assist this process by: actually scheduling these examinations; reviewing the outgoing CE questions and assessing the incoming medical reports; interacting with the medical community to acquaint them with FEC policies and procedures; and enlisting their participation in second opinions and/or referee examinations. The nurse may also coordinate with the DMD/DMA in identifying geographical areas requiring outreach activity and in assisting in the recruiting and retaining of physicians for second opinion referrals.
a. Scheduling Examinations. The use of the Physicians' Directory System (PDS), an automated directory and tracking mechanism, is mandatory in scheduling all referee examinations and is optional in the scheduling of second opinions. Details of this system are found in PM 3-500.7. The nurse should consult FECA PM 3-500.3 and 3-500.4 for the procedures to be used in scheduling second opinion and referee examinations respectively.
The CE determines the need for these examinations and prepares a list of questions to be answered by the examining physician. He or she should indicate the type of specialist required. Claimants are to be scheduled as close to home as is feasible (25 miles is considered reasonable in most urban areas). In rural areas, and in some urban areas with shortages of physicians, the claimant will have to travel over 25 miles.
b. Reviewing Outgoing Material. The nurse may review outgoing material for comprehensiveness of medical data and clarity of the questions posed by the CE. He or she may recommend changes and discuss issues with CE as necessary.
c. Tracking Second Opinion and Referee Examinations. Usually, 30 days is a sufficient time period after the second opinion or referee examination for the specialist to submit the report. Follow-up phone calls should be made in cases where no report has been received in the office within 30 days of the examination. Once received, the report should be reviewed in light of several factors:
(1) Timeliness is an important consideration in the assessment of the quality of medical reports. District offices may set their own criteria in this respect or use six weeks as the standard. Reports that are not timely should be noted in the NOTES section of the PDS for monitoring purposes. If the physician is late in submitting the report, the nurse contacts his or her office and appraises him or her of this fact and obtains a copy of the report as soon as possible. However, if no report is forthcoming after a reasonable waiting period, the nurse notifies the CE for further action.
(2) Content is also crucial. When the report does not address all questions posed by the CE, or contains equivocal answers, the nurse so notifies the CE. Upon request of the CE, the nurse may notify the physician's office of these deficiencies and request clarification or completion of the report. This second request is also tracked and reimbursement for the examination may be withheld until clarification is obtained.
Back to Chapter 3-0201 Table of Contents
12. Supervising Field Nurses. The Staff Nurse is responsible for procuring, training and managing Field Nurses who will work directly with OWCP claimants in the return to work effort.
a. Procurement and Selection. The Staff Nurse develops a structure and a timetable for the procurement and selection of Field Nurses taking into account the geographic, volume, and operational requirements of the district office.
(1) Once the number and location of the Field Nurses needed has been determined, the Staff Nurse solicits the services of nurses through advertisements placed in local newspapers, occupational health journals or other nursing newsletters. Advertisements may also be distributed to local hospitals, universities, nursing schools and vocational rehabilitation companies. A sample advertisement to procure contact nurse services is included in Exhibit 3.
(2) Field Nurses must be selected according to standard criteria which include educational background, licensing, clinical experience, medical case management, and specific workers' compensation or occupational health experience. Selection criteria guidelines are detailed in Exhibit 4.
(3) All applicants should be appraised by the Staff Nurse and any other staff designated by the district office. The appraisals and the reasons for the selections must be well documented by the Staff Nurse.
(4) After the selection of candidates, the Staff Nurse ensures that each receives and signs a memorandum of agreement. The document details the various responsibilities of the nurse and the time frames within which he or she is to accomplish them. The agreement also details the nurse's hourly professional and administrative reimbursement.
b. Training Field Nurses. Most commonly training of Field Nurses is done at the district office location. The training for nurses contracted for this project should not exceed one and a half days since there is no effective way to reimburse them for their time. One day should be devoted to discussing various FEC policies and procedures and one half day should be allocated to addressing the nurse functions (report compliance and completion, billing forms and coding schemes).
In those areas where travel by the Field Nurse to the district office would require several hours or necessitate air travel, the Staff Nurse may wish to consider travel to cities where the Field Nurses are located. The length of training and the agenda topics should be the same. A suggested training outline has been enclosed as Exhibit 5.
c. Managing Field Nurses. Once Field Nurse selections have been made and memoranda of agreements have been signed, the nurse's name, phone and address need to be recorded into the Nurse Tracking System, where available, or into a manual log.
(1) Referring Cases to the Field Nurses.
(a) The Staff Nurse will refer cases to the Field Nurses using geographic rotation. However, sometimes the special needs of the claimant rather than locale may dictate the choice of nurse for a specific case. For example, a claimant with a psychiatric or neurologic disorder would benefit from the intervention of a nurse having this kind of expertise. In this instance, the case would be referred to the nurse having these qualifications rather than to the next nurse on the rotation.
(b) Once the selection is made, a letter which serves as an authorization to perform these services is forwarded to the nurse. This authorization letter reiterates the nurse's functions, responsibilities and reimbursement rate as listed in the memorandum of agreement. The authorization letter also includes the claimant's name as well as all available medical data for use by the nurse in his or her intervention. A sample of this authorization letter may be found in Exhibit 6.
(c) It is recommended that the Staff Nurse maintain a file on each Field Nurse. Data pertaining only to the nurse, e.g. memorandum of agreement, credentials, warnings or assessments of his or her work, can be kept in this folder. Any data pertaining to claimants must be referred to their files.
(2) Field Nurses' Reports. The Field Nurse should complete the Initial Evaluation Form, as shown in Exhibit 1, and return it to the Staff Nurse within 30 days after initial contact with the claimant and the physician. The Progress Report should be submitted to the Staff Nurse on a monthly basis. However, Field Nurses may submit verbal or written reports at any time to the Staff Nurse if issues needing immediate attention arise.
The Staff Nurse should have reviewed and clarified the elements of each of these reports during the Field Nurse training session. It may prove useful to review these data elements again when the case is referred. A supply of these forms may be included in the initial authorization packet or sent to the Field Nurse under separate cover with instructions for completion.
(3) Warning and Termination Procedures. The memorandum of agreement with FEC identifies the responsibilities of the Field Nurse. When any of these responsibilities are not fulfilled by the Field Nurse, the Staff Nurse needs to take immediate corrective action.
For example, the nurse's reports are consistently late or there has been no follow up either by phone or in person with the treating physician. Such delays may hamper possible return to work opportunities. The staff nurse needs to issue verbal warnings to the field nurse after the first two violations, issue written warnings to the field nurse after the second two violations, and terminate the field nurse's working relationship with OWCP after the fifth violation, ensuring that there has been 30 days' prior written notice.
Back to Chapter 3-0201 Table of Contents
13. Other Medical Management Functions of the Staff Nurse. While the primary function of the Staff Nurse is to coordinate nurse services, there are other medically related activities which require his or her expertise. These areas include:
a. Complex Medical Bills. The automated enhancements to the medical bill processing system will suspend bills for a variety of medical issues. The nurse may be called on to evaluate such issues as: assessing the relatedness of a procedure to the accepted condition; clarifying the need for continued prior authorized services (physical therapy, TENS units, home nursing services); resolving excessive charges submitted by consultant physicians; and performing random quality control reviews of bills after payment approval.
b. Training on Medically Related Issues. The nurse may offer training to CEs and other district office staff on an as-needed basis using any of the following methods:
(1) A one-on-one session would be appropriate at the time a CE requested information pertaining to a treatment modality, i.e., a specific drug, diagnostic examination or operative procedure.
(2) An informal group session may prove helpful if the nurse is approached by a Supervisory CE (SCE) to assist the module in a specific issue, e.g., formulating the questions posed to treating, second opinion and referee physicians.
(3) Formal group sessions may be organized when the nurse identifies the expertise of a medical consultant, either in-house (DMD/DMA) or from outside the Office, and arranges for that doctor to discuss his or her specialty with the CEs and other office staff. Training by the nurse may also be initiated with new DMDs/DMAs, contact representatives and office staff resolving bill problems.
Back to Chapter 3-0201 Table of Contents
14. Billing by the Field Nurse. Billing periods are to correspond to the report (either Initial or Progress) service periods, i.e., monthly, and the program will not accept bills that arrive without a report. A bill must not contain charges for services that fall outside the billing period or for unpaid balances from prior billing periods.
a. The following requirements must also be met for reimbursement approval:
(1) Form. The only acceptable billing form will be the HCFA-1500.
(2) Codes. Only the specific internal codes with appropriate terminology and dollar amounts designated for professional and non-professional services will be acceptable.
(3) Submission of Bills. A HCFA-1500 needs to be completed in duplicate for each claimant receiving nursing service. A duplicate report (initial/progress) must also be attached to the duplicate HCFA form. The words "PROMPT PAY" should be written at the top and bottom of the original HCFA billing form. The envelope should also be marked "PROMPT PAY" to the attention of a designated individual. A sample of a correctly completed HCFA-1500 form is shown as Exhibit 7 (Link to Image).
Back to Chapter 3-0201 Table of Contents
15. Functional Capacity Evaluations (FCEs). These evaluations may be classified in two types according to their purpose, duration and content: a general-purpose FCE, and an FCE for placement into an Occupational Rehabilitation Program (ORP) such as Return to Work or Work Readiness (commonly called work-hardening, work conditioning, etc.)
a. A CE or SN may authorize a general-purpose FCE in cases where management of disability calls for clarification of job tolerances, job modifications, etc., and the treating physician, second opinion or referee specialist recommends or requires this service. However, only a Rehabilitation Specialist can authorize an FCE in connection with an ORP (see PM 2-813).
b. Before authorizing the FCE, the CE or SN should review the case and verify that the injury occurred more than three months ago, the functional impairment is of moderate to high complexity, and the services recommended by the physician exceed routine physical performance tests and measurements (e.g. CPT 97750). More detailed guidelines appear in Chapter 1 of MEDGUIDE.
c. The CE or SN advises the recommending physician that the FCE is approved. Based on the severity of the case and whether or not any complicating factors are present, up to eight hours can be approved for a general-purpose FCE.
d. The CE or SN completes the authorization form and enters the authorization in the "Notes" section of the Case Management File (CMF). To ensure the accurate processing of bills for the FCE, the following information must be included: the approved service code, the number of hours approved, the name of the provider, and, as necessary, the use of modifiers.
The CE or SN also notifies the Field Nurse (FN) assigned to the case of the authorization of the FCE and provides the FN with a copy of the authorization.
Back to Chapter 3-0201 Table of Contents
Exhibit 1: Initial Evaluation of Claimant
|
TO: NAME OF CE OR COORDINATOR |
File #: |
|
FROM: NAME OF NURSE |
ICD Accepted |
|
PHONE #: NURSE'S TELEPHONE NUMBER |
|
|
Claimant Name: |
Address: |
|
Primary Physician: |
Address: |
|
Phone: |
|
|
Employer: |
|
A. PERSONAL INFORMATION
Family Dynamics and Home Situation (detail only those factors which relate to claimant's return to work):
B. JOB HISTORY
Description of Injury (including date of injury):
INITIAL EVALUATION OF CLAIMANT, Continued
C. MEDICAL HISTORY
Current Medical Status (include consulting physicians)
History of Previous Injuries
Non-Injury-Related Medical Conditions
Current Medications
Physician(s) Contacts/Conclusions
D. NURSING CARE PLAN
Potential Problems
Recommendations
Planned Services During the Next 30 days
Planned On-site Visit to Agency/Work Site
Back to Chapter 3-0201 Table of Contents
Exhibit 2: Progress Record
|
Report Date: |
|
|
Claimant Name: |
Case File #: |
|
Claimant Address: |
ICD Accepted |
|
Name of Nurse: |
Phone: |
A. DATES OF SERVICE
|
From: |
To: |
B. SUMMARY OF PROGRESS TO DATE
C. ACTIONS TAKEN DATES
D. NURSING CARE PLAN
|
Planned Services For the Next 30 Days
|
|
|
Potential Problems |
Recommendations |
Back to Chapter 3-0201 Table of Contents
Exhibit 3: Sample Advertisement for Nurse Services
The U.S. Department of Labor, Federal Employees' Compensation Program (FEC) is currently seeking to contract with nurses to work with claimants and their treating physicians to coordinate treatment, promote recovery and ultimately facilitate the return to work of the claimant.
An applicant must have the following minimum qualifications to be considered for this service: a registered nurse (R.N.) license; at least two years of general medical-surgical clinical experience; and at least two years of case management experience. Additional expertise desired includes: a basic knowledge of workers' compensation injuries and illness; excellent oral and written communication skills; good organizational and time-management skills, and proven decision-making abilities. Selection will be based on the combination of education and expertise that best meets the needs of the Department of Labor.
The hourly rate for a contract registered nurse is $00.00 for professional services and $00.00 for administrative services.
If you wish to pursue this opportunity, please submit your curriculum vitae showing the qualifications as listed above, along with a copy of your current nursing license to:
DISTRICT OFFICE ADDRESS
All applications must be received in this office no later than DATE.
If you need further information, you may contact:
NAME, TITLE AND PHONE NUMBER
OF DISTRICT OFFICE CONTACT
Back to Chapter 3-0201 Table of Contents
Exhibit 4: General Selection Guidelines
General Selection Guidelines
Describe qualifications under the following categories:
A. Nursing Degree (R.N.) License Number____________
B. Clinical Experience Dates
Specialty
General Medical-Surgical
Emergency
Critical Care Unit (CCU, ICU, etc.)
Other
C. Positions Held Dates
Staff Nurse
Team Leader
Head Nurse
Other
D. Additional Experience Factors
- demonstrates in the C.V. that he/she has medical case
management experience.
- shows workers' compensation case experience through past
positions held, e.g. with DOL, State or private sector carrier.
Back to Chapter 3-0201 Table of Contents
Exhibit 5: Suggested Training Topics
SUGGESTED TRAINING TOPICS
A. Introduction
- Overview of Nurse Intervention
- Objectives of the Training
B. Training Outline
The Federal Employees' Compensation Program: CA-810 and CA-550
1. Coverage of FECA
- Constituency (variety of occupations)
- Kinds of Claims--traumatic,occupational diseases
- Kinds of Benefits--compensation, medical, vocational rehabilitation etc.
- Philosophy of the program--non-adversarial
- Organization of program; geographical distribution, district office structure
2. How claims are adjudicated and managed (brief description)
- Notice of Injury
- Forms CA-1 and CA-2
- Acceptance, ICD diagnoses codes
- Continuation of Pay
- Compensation, short/long term
- Reemployment and Vocational Rehabilitation
3. Nurse Intervention Process
- Roles/responsibilities
- Reporting Mechanisms
- Claimant/Physician Communication
- Billing Procedures
- Security of Files
- Schedule for additional training/problem-solving sessions
4. Tour of the District Office
Back to Chapter 3-0201 Table of Contents
Exhibit 6: Sample Letter Authorizing Nurse Services
|
Case File #: |
Dear NAME OF NURSE:
This letter serves as a referral and authorization to you to provide medical management services to the above-named injured worker. It also serves as notification that you may contact the treating physician to coordinate the medical treatment, and the employing agency to clarify the requirements of the injured worker's job. As previously discussed, your hourly rate will be $00.00 for professional services and $00.00 for non-professional charges. There is a $3,000 or 60 hours of nursing service maximum limit per case. On an exception basis, one extension only can be authorized, so that the total services per case may not exceed 120 hours or $6,000.
In case(s) assigned to you, your responsibility will be to communicate directly with the injured worker and his/her family as deemed necessary to explain and monitor medical treatment and progress. As needed, you will obtain concrete work limitations and communicate directly with physician and agency about light duty opportunities.
Enclosed is a summary of case information and the significant medical reports for your official and confidential use. This information must be kept in a secure location which only you have access to. When the case is closed, please return the case information to this office. The case information supplied to you is the property of OWCP and cannot be discussed with parties other than the claimant, (claims examiner/ coordinator), physician and employing agency.
Should you have any questions or comments regarding the contents of this letter, please contact NAME OF CE OR COORDINATOR on PHONE NUMBER.
Sincerely,
STAFF NURSE
Back to Chapter 3-0201 Table of Contents
Exhibit 7: Prompt Pay Authorization (Link to Image)
Back to Chapter 3-0201 Table of Contents
|
Paragraph and Subject |
Date |
Trans. No. |
|---|---|---|
|
Table of Contents |
03/95 |
95-12 |
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
Exhibits |
Date |
Trans. No. |
|---|---|---|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
3. Scoring Instructions for Contract Field Nurse Applications |
03/95 |
95-12 |
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
|
|
03/95 |
95-12 |
1. Purpose and Scope. The program uses contract field nurses to perform nurse intervention in Quality Case Management (QCM) cases as well as in other case management initiatives. This chapter describes and standardizes the Office of Workers' Compensation Programs' (OWCP's) procedures for soliciting, recruiting and selecting contract field nurses.
In addition, the chapter also defines the role of the staff nurse in managing and tracking the activities of the contract field nurse.
Each district office will contract with the specific number of nurses which have been identified as the number needed to adequately serve the injured workers within a specific geographical area. The staff nurse will act as the coordinator at the district office level. The National Office will assist in the certification process by coordinating the solicitation for contract nurses on a national basis, sending out the application packet to applicants and responding to certification questions or concerns raised by the staff nurse or other individuals.
Back to Chapter 3-0202 Table of Contents
2. Certification Process. The certification process provides for a standardized approach for procuring the services of contract field nurses. This process consists of soliciting, recruiting, selecting and contracting with registered nurses to work with claimants. The contract or memorandum of agreement is valid for a period of two (2) years. After this initial period, field nurse services may be renewed yearly for three option years. National certifications of field nurses occur at five (5) year intervals, however the individual district offices may hold local certification drives when needed. The staff nurse determines that additional field nurses are necessary to fulfill specific needs when:
a. Field nurses voluntarily withdraw from OWCP's program and need replacement.
b. The number of claimants requiring the services of a field nurse increase in a certain geographic area.
c. The performance of a field nurse (late reports, refusing case referrals) may prompt the staff nurse to discontinue referrals to particular nurses and require additional recruitment.
d. Option year attrition occurs.
Once the need for a local certification drive is established, the district office submits a memo requesting additional field nurses to the Chief, Branch of Medical Standards (BMSR) in the National Office for consideration. The letter must contain: the anticipated dates and location of the training, the geographic areas involved by zip code clusters, and the number of field nurses needed to satisfy the additional need. After the request is approved, the Chief, BMSR, determines the schedule for the additional certification training workshop and ensures the availability of adequate support resources.
Back to Chapter 3-0202 Table of Contents
3. Field Nurse Allocation. The FEC staff nurse (SN) in each district office determines the number of field nurses (FN) needed for each geographical area and reports the number to BMSR. The staff nurse may use the same allocation or clustering established for the vocational rehabilitation counselors. A cluster consists of a number of adjacent zip codes grouped together based on reasonable size, ease of travel within the cluster, and the number of claimants located within this area. Once the geographic unit or cluster is established, automated reports detailing the number of claimants residing in the cluster can be obtained. The staff nurse uses this information and her own experience to establish the number of nurses needed in the cluster. This number is then reported to BMSR.
Back to Chapter 3-0202 Table of Contents
4. Recruitment. Solicitation for the services of registered nurses to perform contract field nurse activities is made both at the National and District Office levels.
a. The Chief, Branch of Medical Standards and Rehabilitation (BMSR), places the advertisement in the Commerce Business Daily and in other selected national publications (ANA newsletter, National Black Nurses' Association newsletter, etc.)
b. The district office conducts advertisement at the regional level in local nursing organization newsletters, and newspapers. The names of nurses who have previously expressed interest in joining the program should be maintained in a file so that they are included in the district office solicitation. Field nurses who are currently certified also need to be mailed a copy of the advertisement by the district office.
c. The advertisement contains the minimum qualifications required, the geographical region(s) for which the field nurses are needed, instructions for responding and a response due date. If the district office plans to conduct interviews as part of the selection process, this also needs to be mentioned in the advertisement.
d. BMSR receives the responses to the advertisement, categorizes these responses by geographic area and distributes a list to the district offices. BMSR sends all timely respondents an application package. Only responses postmarked on or before the due date are processed further; late respondents will be notified that they are not eligible for this certification but will be notified when an advertisement is placed for the next certification. The DO staff nurse maintains alphabetically organized late response files for this purpose.
Back to Chapter 3-0202 Table of Contents
5. Nurse Selection Method.
a. The Staff Nurse in each DO acts as the coordinator for the selection process. Upon receipt of the completed application forms (OF-612 is shown in Exhibit 1 (Link to Image)), the staff nurse, or designated district office staff, compiles them by geographic area/cluster, ensuring that only applications received on a timely basis are included. Late applications will not be rated and the applicants will be sent a postcard by the district office explaining the rejection.
b. The Field Nurse Panel evaluates the applications from the field nurses based on pre-determined criteria and selects qualified candidates to be part of the OWCP nurse intervention program. The panel is composed of the district office staff nurse and national office staff. The panel members evaluate each application independently, and then, via telephone, reach a consensus regarding the ranking of the field nurse candidates. As needed, a third panel member may be used in those circumstances when a "tie-breaker" decision is needed.
c. The panel uses the scoring sheets (see Exhibits 3 and 4) to rate each application considering the following factors: work experience in case management, specialized nursing skills, educational background and certifications. The first step in the rating is to verify that the applicant meets the minimum requirements by checking Block 13. If no R.N. license number is listed, or if there is no photocopy of the license attached, the reviewer does not proceed and the applicant is disqualified.
In addition, the other minimum requirements of two (2) years generalized medical/surgical clinical experience and two (2) years in case management or an equivalent (Block 8) need to be clearly indicated in the applicant's work experience. Absent these factors, the applicant is disqualified. An unsatisfactory performance evaluation should be grounds for non-selection.
d. The specific aspects of how to score experience and education are detailed further on the instruction sheet attached to the rating form (see Exhibit 2). Each member needs to obtain a copy of the candidates OF-612 application form and the rating sheet. Data contained on this sheet is self-explanatory. However, it is important to document reasons for disqualifying an applicant. It is also important to indicate the reason(s) for 0 points in any category. When the rating process of an application is completed, panel members total the number of points awarded in each section, sign and date the rating form.
e. Ranking and Selection.
(1) Panel members rank the qualified applicants by the total number of points awarded on the application form, placing the applicant with the most points at the top of the list. In cases where applicants receive identical scores and one is above the cut-off line but the other is not, each is selected for certification.
(2) Once the list is completed, panel members draw a cut-off line so that the number of applicants above the line corresponds to the number of field nurses that the district office wants to certify.
(3) All application materials are returned to the staff nurse coordinator.
(4) The staff nurse takes the applications of those considered qualified and verifies the accuracy of the licenses with the applicable state licensing board for currency and good standing status. In addition, the name and/or company which employs the field nurse needs to be checked against the U.S. General Services Administration (GSA) list of Excluded Parties From Federal Procurement Programs. This monthly publication identifies those parties excluded throughout the U.S. Government from receiving Federal contracts. If the nurse or company employing the nurse appears in the book, the applicant cannot be selected. A field nurse who is not selected for this reason needs to be notified that his or her non-selection was based on this information. The publication can be procured from the regional OASAM office or electronically from G.S.A.
Back to Chapter 3-0202 Table of Contents
6. Interview.
a. At this point in the selection process, the staff nurse may interview those eligible candidates in the office's regional jurisdiction who are within a competitive range. For the purpose of nurse certification, a competitive range is defined as the number of nurses who are qualified and selected plus those who are qualified but not selected. Within this group the staff nurse defines a fair and reasonable number of nurses to interview. To do this, the staff nurse considers her own time constraints and the availability of the candidates. Since an interview is a subjective process, and the points earned from this process should not substantially alter the original rating score. For this reason, the points assigned to an interview should not exceed three (3).
b. The selecting official (staff nurse) has the authority to determine the extent of the competitive range based on a fair and reasonable estimate. For example, if the pre-determined number of nurses for a specific area is 10, and 15 applicants are found qualified, the interview should include all 15. However, if the pre-determined number for an area is 10 and 35 applicants are eligible, it is not reasonable to interview the 25 additional applicants.
c. Questions posed during the interview must:
(1) Be the same for everyone.
(2) Relate to job performance, the strengths/weaknesses the applicant brings to the job, and what is expected of him or her.
(3) Be documented together with the applicant's response.
Back to Chapter 3-0202 Table of Contents
7. Notification to Applicants. At the conclusion of the rating or interview process, whichever is the final selection factor, all nurses are notified of their individual status. Nurses selected for the program are made aware of the selection and given the necessary information on the certification training workshop. Those not selected will be given reasons for this action. Sample acceptance and denial response letters are included in Exhibits 5 and 6.
Back to Chapter 3-0202 Table of Contents
8. Certification Training Workshop. The certification process ends with the training workshop. Throughout the course of the certification process, the staff nurse prepares for the training session. A suggested organizational time table has been developed for the staff nurses' use in planning the workshop and can be referenced on Exhibit 7.
The training will typically last only one day since there is no effective way to reimburse the nurses for their time. The training is divided into two parts: a description of the FEC policies and procedures, and the contract nurse responsibilities (e.g. report compliance and completion, billing forms and coding schemes, etc.) At the completion of the Certification Workshop the staff nurse ensures that all newly certified field nurses sign and date a new memorandum of agreement. It is at this expiration date that the option years begin.
It may be necessary to conduct the workshop more than once if the number of nurses is very large or if the geography is such that prolonged travel is required to reach the city where the training is held.
Back to Chapter 3-0202 Table of Contents
9. Option Year Renewal. On each option year the staff nurse will need to decide whether to renew the services of each field nurse. To do that, the staff nurse reviews the field nurse's work performance in terms of timeliness, quality, billing characteristics, intervention successes, compliments or complaints received from employing agencies, claimants, FEC staff, presence or absence of verbal and/or written warnings. This yearly evaluation is a composite of all the case-related evaluations performed when a case is either closed or transferred to another field nurse. A sample of this evaluation is found on Exhibit 8. Each field nurse is notified by letter as to whether his or her contract was renewed or not for the option year.
If the contract is renewed, the field nurse signs another memorandum of agreement providing the staff nurse with updated information (R.N.license expiration date, home address/phone changes). The staff nurse also assesses whether another training (abridged) session is necessary. Applicants will be notified if a training session is planned. BMSR also needs to be made aware of the training schedule.
Back to Chapter 3-0202 Table of Contents
10. Contract Field Nurse Management. Staff nurses will be responsible for the managing of contract field nurses within their geographical jurisdiction. The staff nurse will: maintain all manual and automated records referring field nurses, generate case referrals, supervise their work performance and provide them with periodic reviews, reserving the authority to terminate those field nurses whose performance is not in keeping with OWCP policies and procedures. A more extensive explanation of the staff nurses responsibilities in managing the field nurse activities may be found in the FECA PM Chapter 3-0201.
Back to Chapter 3-0202 Table of Contents
11. Referring Cases to the Field Nurses.
a. The staff nurse will refer cases sequentially to the field nurses using a geographic rotation. The district offices may use an automated system, i.e., Rehabilitation Tracking System (RTS), Nurse Tracking System (NTS) or maintain the rotation through use of a manual log.
The rotation is based on a geographic match between the first three digits of injured worker's zip code and that of the field nurse. Ideally, the field nurse should be located within 25 miles of the injured worker's residence but may be located as far away as 50 miles. If there are no available field nurses within a 50 mile limit, the staff nurse may refer the case to the field nurse having the best method of access to the injured worker even if that nurse is located in a different zip code area. This situation typically occurs when the injured worker is on the border of one geographic cluster, it may be more efficient in time and money to assign a field nurse from a different zip code range or cluster since it is closer geographically.
b. Sometimes the special needs of the claimant rather than locale may dictate the choice of a nurse on a specific case. When a particular case requires special skills or knowledge that the next field nurse in sequence does not possess, the staff nurse may select the field nurse out of sequence. Documentation as to the reason for not following the rotation needs to be maintained in whatever system is in use (manual or automated system) in the district office.
c. Once the case assignment is made, a letter which serves as an authorization to perform these services is forwarded to the field nurse. This authorization letter reiterates the nurse's functions and responsibilities as listed in the memorandum of agreement. In addition to the authorization letter, the field nurse will also receive relevant CA forms, all available medical data (reports and objective findings) and the Form OWCP-5.
d. The staff nurse maintains a file on each field nurse. Data pertaining to the nurse such as a copy of memorandum of agreement, credentials, warnings and/or assessments of his or her work can be kept in this folder.
Back to Chapter 3-0202 Table of Contents
12. Tracking the Field Nurse Intervention. Using the data described below, the staff nurse will be able to analyze various aspects of the program and obtain the basic statistics necessary to manage the nurse intervention effort. These statistics include: the number of claimants and nurses participating in the intervention program at any given time, the duration and result of the intervention by case or in a cumulative fashion, the rotation of cases among the field nurses and other data.
a. Claimant Data. From the moment a claimant is selected for nurse intervention, data is entered by the CE on the QCM screen. The staff nurse will also enter information on the name of the field nurse and the date the case was referred out. A return to work date is also captured on this screen.
b. Field Nurse Data. Information regarding the field nurses should also be maintained including the name of each nurse, home address, phone number and geographical location.
Back to Chapter 3-0202 Table of Contents
13. Warning and Termination Procedures. The memorandum of agreement with OWCP identifies the duties and responsibilities of the field nurse. When any of these responsibilities are not fulfilled by the field nurse, the staff nurse needs to take immediate corrective action in the form of a warning. At any point in the warning/termination process, the staff nurse may opt to decrease the workload of the field nurse as an incentive for a change in behavior. The decrease in workload needs to be documented and maintained only for a finite time period. If the field nurse's work improves, she is restored to the rotation. If there is no improvement, the staff nurse proceeds with the verbal warnings. If there is a serious violation of ethics such as breach of confidentiality, falsifying documents or other fraudulent activities, dismissal is immediate.
The staff nurse needs to document each stage of the termination process by entering the date and type of violation and the date and type of staff nurse response (verbal warning, final letter etc.)
a. Verbal Warning. The staff nurse may issue a verbal warning when the field nurse demonstrates a lack of professionalism or violates any of the conditions in the memorandum of agreement.
b. First Termination Warning Letter. The staff nurse will send the "First termination warning letter" after he/she has issued a verbal warning within a twelve-month period and the field nurse continues to demonstrate a lack of professionalism or violates the conditions of the memorandum a second time. Copies of this letter are placed in the field nurse's file.
c. Final Termination Letter. The staff nurse will send a termination letter when the field nurse continues to demonstrate a lack of professionalism or violates conditions of the memorandum again within twelve months after receiving the first termination warning letter. The staff nurse calls the field nurse and advises that, as of the date of mailing, no further services should be provided or billed for because his or her cases have been transferred to another field nurse. A copy of this letter is also placed in the field nurse's file and sent to the Regional Director and Chief, BMSR.
d. Reconsiderations and Appeals. The field nurse may request a reconsideration or appeal within 30 days after receiving a termination letter or, in the case of appeals, a reconsideration decision. A reconsideration request should be accompanied by relevant evidence to support the field nurse's arguments. The Regional Director will decide all reconsiderations within 90 days of receiving the request. The Director, Planning, Policy and Standards Division in the OWCP's National Office will decide all appeals based on the evidence of record within 90 days of receiving the request.
Back to Chapter 3-0202 Table of Contents
Exhibit 1: Optional Form (OF) 612 Application Form (Link to Image)
Back to Chapter 3-0202 Table of Contents
Exhibit 2: Completion Instructions For Optional Form 612
INSTRUCTIONS TO APPLICANTS:
This application form is being forwarded to you in response to the OWCP solicitation to contract with registered nurses for early intervention of injured employees.
Please complete only those items listed below and return to (Name/Address of the District Office) postmarked no later than (Insert Date).
The information which you submit on this OF-612 Application Form will be compared to the minimum requirements developed by OWCP for contract field nurses. The minimum requirements are:
1. Evidence of two years' specialized case management experience (experience can be in workers' compensation, occupational or community health, utilization review, discharge planning or rehabilitation nursing (Block 8).
2. Evidence of two years' general med-surgical clinical experience (Block 8).
3. Evidence of a valid, current R.N. license. Your R.N. license number(s) needs to be present in Block 13 or a photocopy of the license needs to be attached to the application.
4. All applications must be accompanied by your latest performance appraisal. If this appraisal is more than five years old, please submit three letters of reference from three clients (employers).
Failure to meet the above requirements or to return the form by the deadline date will result in disqualification of your application.
|
ITEM NO. |
EXPLANATION |
|---|---|
|
4, 5, 7 |
Personal data--self-explanatory. |
|
6 |
Applicant's home address (NOT employer's). |
|
8 |
(Include prior work with OWCP) In describing your most recent work experience, CLEARLY indicate evidence of: (1) case management skills (identify experiences in workers' compensation, occupational or community health, utilization review, discharge planning, rehabilitation nursing. (2) at least two years in general med-surgical nursing. (3) any specialized clinical nursing expertise e.g. ICU, CCU, neurology, orthopedics, psychiatry. Additional sheets may be used if necessary |
|
10-12 |
Educational Data. Self-Explanatory. This section must at a minimum indicate that applicant attained: Associate Degree, Diploma or Bachelor's Degree. Graduate level degrees will be awarded points on the highest level of college work completed. |
|
13 |
Other Qualifications. ** At a minimum this block MUST contain an R.N. license number(s) or a photocopy of the R.N. license must be attached. If this info is missing, applicant is disqualified. Additional items to address in this area include: (a) when applicable, certification credentials, e.g. COHN, CCM, CIRS etc. (b) special skills when applicable e.g. psychiatric, catastrophic nursing expertise. |
|
18 |
Signature. |
Back to Chapter 3-0202 Table of Contents
Exhibit 3: Scoring Instructions for Contract Field Nurse Applications
SCORING INSTRUCTIONS FOR CONTRACT FIELD NURSE APPLICATIONS
Introduction
These sheets will be used by the reviewer to score the applicant's information submitted on the Optional Form (OF) 612 and supplemental sheets.
Information on the OF-612 will be compared to the minimum requirements developed by OWCP for contract field nurses. The minimum requirements are:
1. Evidence of two years' specialized case management experience (experience can be in workers' compensation, occupational or community health, utilization review, discharge planning or rehabilitation nursing). (Block 8)
2. Evidence of two years' general med-surgical clinical experience. (Block 8)
3. Evidence of a valid, current R.N. license. R.N. license number needs to be either present in Block 13 or a photocopy of the license needs to be attached to the application.
4. The latest performance appraisal. If this appraisal is more than five years old, three letters of reference from three clients (former employers) MUST also be enclosed.
In scoring the application, it is important for the reviewer to first check to see if the work experiences indicating case-management and med-surgical expertise as well as the R.N. License Number/photocopy of license are present. If any of these factors are NOT present, the candidate is disqualified and no further review of the application is necessary.
Back to Chapter 3-0202 Table of Contents
Exhibit 4: Scoring Sheets
SCORING SHEETS
The following three items reflect the minimum requirements and must be clearly indicated on applicant's form. If any of the three items are not present, discontinue your review, applicant is disqualified.
|
Block # |
Data |
Score |
|
8 |
Review for Specialized Experience |
N= 0 |
|
If 2-3 years' experience |
2 |
|
|
Review for Med-Surg Experience |
N= 0 |
|
|
If 2-3 years' experience |
2 |
|
|
13 |
Check for R.N. license numbers |
N= 0 |
|
The additional items are to be scored in addition to the above requirements. |
||
|
4-7 |
Personal Data |
N= 0 |
|
8 |
Work Experience |
|
|
Review for previous work with OWCP |
|
|
|
- reports/communication timely & complete |
Y= 1 |
|
|
- billing accurate & timely (85%) |
Y= 1 |
|
|
- works well with claimants, staff, physicians, employing agencies |
Y= 1 |
|
|
- no previous OWCP work experience |
N= 0 |
|
|
Review for additional areas of clinical expertise in any of these areas, |
||
|
If 1-2 years' experience |
1 |
|
|
10-12 |
Educational Background-- |
|
|
Review for evidence that applicant earned at least one: |
2 |
|
|
Additional points will be given for the highest level of college work completed, e.g.: |
1 |
|
|
13 |
In addition to R.N. license number(s), Other Certifications related to case management may be entered here, e.g., No additional points will be given for this now but at next certification additional points will be given. |
|
|
Total Points= |
Name of Reviewer __________________________
Date of Review ____________________________
Back to Chapter 3-0202 Table of Contents
Exhibit 5: Sample Response To Field Nurse--Acceptance
Dear FIELD NURSE:
I am pleased to accept you as an OWCP contract field nurse. To complete the certification process, a training workshop is planned for:
DATE:________________
TIME:________________
PLACE:_______________
Please detach and return the lower portion of this letter to me at the above address. Your workshop reservation must be postmarked by the following date:_______________
You may contact me at __-__-__ if there are any questions on this workshop.
Sincerely,
STAFF NURSE
_____________________________________________
___ I will attend the workshop. ___ I will not attend the workshop.
Please print your name:
_________________________
Home Address:
Back to Chapter 3-0202 Table of Contents
Exhibit 6: Sample Response To Field Nurse--Denial
Dear FIELD NURSE:
Thank you for your interest in the Office of Workers' Compensation Programs' (OWCP's) nurse intervention program. As a result of the certification process, I am unable to select you to provide services to OWCP injured workers for the reason (s) indicated below:
_____You are qualified for selection. However, we selected the maximum number of field nurses needed to provide services within the geographical area of the District Office. You may be selected at a later date if we have a need for new field nurses.
_____Your application did not meet our minimum qualifications based on either case management and/or med-surgical clinical experience.
_____Your application was incomplete.
Your response to our solicitation for contract field nurses to provide services to our injured workers is appreciated.
Sincerely,
STAFF NURSE
Back to Chapter 3-0202 Table of Contents
|
WEEKS TO WS |
ACTION |
STATUS |
|---|---|---|
|
10 weeks |
1. Determines the number of or earlier field nurses, presents geographic distribution plan to RD, NO. 2. Advertises Contract Field Nurse Position in local nursing journals, newsletters, newspapers etc. 3. Coordinates date and location of the workshop with DO and NO. |
|
|
9 weeks |
1. Confirms attendance of district and NO staff (BMSR) who will deliver welcoming and closing remarks, as well as part of the actual training. 2. Reserves space for the workshop, preferably in a Federal Building. 3. Ascertains that all necessary furniture, equipment, and supplies will be available. |
|
|
7 weeks |
1. Rejects incomplete applications. 2. Refers completed forms to panel for evaluation and ranking. 3. Organizes application materials after panel completes selection. 4. Creates folder for "Selected" Applicants. 5. Creates additional folders marked "Qualified-Not Selected" and "Disqualified" Applicants. |
|
|
5 weeks |
1. Completes/mails acceptance letter or earlier which includes date/time/place of training workshop. Include to whom form should be returned and by what date (should be no later than three weeks before the workshop). 2. Sends notification to the "Qualified-Not Selected" and "Disqualified" applicants. |
|
|
2 weeks |
1. Compiles training materials, draws up final agenda, sends this information to BMSR for concurrence. 2. Makes sure all available spaces for the workshop are filled. 3. Prepares Workshop Attendance Log. 4. Contacts FNs who did not respond to the letter and verify their attendance. 5. Notes the reason for non-attendance on the log and replace with field nurses from the "Qualified-Not Selected" folder. |
|
|
Day Before Workshop facility |
1. Checks the physical location and set-up of the training 2. Reminds speakers of the time/place of the workshop. |
|
|
Workshop Day |
1. Supervises the sign-in procedure for attendees. 2. Distributes materials and acts as resource person. 3. Conducts sessions. 4. Ensures all participants complete and sign a Memorandum of Agreement. 5. Checks that each participant has provided you with his or her phone number and home address. |
|
|
After Workshop |
1. Ensures that all pertinent FN information is entered on either the RTS or district office tracking system. |
Back to Chapter 3-0202 Table of Contents
Exhibit 8: Contract Field Nurse Evaluation Form
CONTRACT FIELD NURSE EVALUATION FORM
F.N.'s Name:_____________________________________________
I.W.'s Name:_____________________________________________
Claim File:_______________________________________________
________________________________________________________
Instructions: This evaluation form should be completed when the FN submits the closure report or when the case is assigned to another field nurse or transferred to another district office.
|
Did the FN: |
Yes |
No |
N/A |
1. Respond timely to the request for case referral?
2. Communicate timely and effectively with IW, AP, EA, SN, CE and other parties?
3. Identify problems which could affect the RTW promptly and accurately?
4. Offer good problem-solving techniques and/or offer viable recommendations to OWCP?
5. Only make commitments based on the written approval and authorization of OWCP?
6. Provide and coordinate necessary services (e.g., schedule of second opinion exams) without delay?
7. Follow the directions of the SN and CE?
8. Submit reports and bills timely and accurately?
Back to Chapter 3-0202 Table of Contents
|
Paragraph and Subject |
Date |
Trans. No. |
|---|---|---|
|
Table of Contents |
2/12 |
12-05 |
|
2/12 |
12-05 |
|
|
2/12 |
12-05 |
|
|
3. Form CA-16 Authorization for Examination and/or Treatment |
2/12 |
12-05 |
|
2/12 |
12-05 |
|
|
2/12 |
12-05 |
|
|
6. Transfer or Termination of Authorization for Medical Care |
2/12 |
12-05 |
1. Purpose. An injured employee is entitled to receive all medical services, appliances or supplies which a qualified physician prescribes or recommends and which OWCP considers necessary to treat the work-related injury. The purpose of this chapter is to describe the circumstances under which OWCP or, in some instances the employing agency, may authorize medical services for injured claimants. See 5 U.S.C. 8103.
Back to Chapter 3-0300 Table of Contents
2. Requests for Authorization. While claims personnel may receive a request for examination and treatment, the majority of such requests are received initially by the Office of Workers' Compensation Programs' (OWCP) designated bill processing agent.
a. Types of Treatment Requested.
(1) Routine Medical Care Routine medical services such as office visits, physical therapy, and requests for durable medical equipment are reviewed by OWCP and its designated bill processing agent to determine whether the treatment is consistent with the accepted work related conditions. If the treatment can be approved, an authorization letter is issued. If the treatment cannot be authorized, the requestor may submit further medical documentation for consideration.
(a) Any qualified physician or qualified hospital may provide such services, appliances and supplies. Non-physician providers such as physicians' assistants, nurse practitioners, and physical therapists may also provide authorized services for injured employees to the extent allowed by applicable Federal and State law, but this does not include certification for periods of disability, unless such is provided with the concurrence of a physician. See 20 CFR 10.310.
(b) A clinical psychologist may serve as a physician only within the scope of his or her practice as defined by State law. Therefore, a clinical psychologist may not serve as a physician for conditions that include a physical component unless the applicable State law allows clinical psychologists to treat physical conditions. A clinical psychologist may also perform testing, evaluation and other services under the direction of a qualified physician.
(c) A specialist in the field of occupational medicine can serve as a treating physician and prescribed treatment may be authorized. As a sub-specialty under the Board of Preventive Medicine, occupational medicine physicians are specialists in the field of workplace injuries and illnesses and their causal associations. They also specialize in assessing an employee's ability to work.
(2) Emergency. If an emergency exists, the Claims Examiner (CE), in consultation with a District Medical Advisor (DMA) as needed, may authorize treatment. Otherwise, the requestor should be advised that the physician should submit a written request detailing the type of treatment recommended and the reason it is needed.
Authorization is sometimes requested for a non-emergency procedure scheduled for the immediate future. If the authorization cannot properly be given by the date in question, the requestor should be asked to submit a written request as described above and advised that if the request is approved, payment may be authorized after the fact.
(3) Surgery. Authorization for surgery should be obtained in advance whenever possible in order to ensure payment. Even if surgery is undertaken without OWCP approval, however, the cost may be reimbursed if the procedure is later found to be acceptable. See FECA PM 2-0810 and 3-0400 for a description of the criteria used to determine if surgery should be approved.
(4) Chiropractic Services. Services of chiropractors that may be reimbursed are limited by the Federal Employees' Compensation Act (FECA) to treatment for the correction of spinal subluxation. The costs of tests performed by or required by a chiropractor to diagnose such a subluxation are also payable. A chiropractor may also provide services in the nature of physical therapy, but only under the direction of, and as prescribed by, a qualified physician. See 20 CFR 10.311.
(5) Attendant Services. Attendant services will be considered for payment as long as the personal care services have been determined to be medically necessary and are provided by a home health aide, licensed practical nurse, or similarly trained individual, subject to requirements specified by OWCP. OWCP will pay for the services of an attendant under section 8103 of the Act, instead of section 8111(a). See 20 CFR 10.314. Note that any existing attendant allowance payments made under 5 U.S.C. 8111(a), initiated prior to January 4, 1999, will continue.
b. Contractual Obligation. Authorization by OWCP for medical examination and/or treatment constitutes a contractual agreement to pay for the services if the services are rendered, regardless of whether a compensable injury or condition exists. Moreover, any medical condition resulting from authorized examination or treatment (such as residuals from surgery) may form the basis of a compensation claim for impairment or disability, regardless of the compensability of the original injury. For both of these reasons, great care must be exercised in authorizing medical examination and/or treatment. See Frederick J. Williams, 35 ECAB 805 (1984) [Where appellant's official supervisor authorized appellant's examination by the Medical Center on the date of the alleged injury, this created a contractual obligation to pay for the cost of this examination regardless of the ultimate action taken on the claim.]
c. Documentation. A CA-110, Report of Call, or a memorandum to the file must be completed by the CE to document all telephone calls concerning authorization or denial of examination and/or treatment. Usually, however, an authorization letter is issued by OWCP's designated bill processing agent.
Copies of letters of authorization addressed to physicians and medical providers are not usually sent to the employing agency. They may be provided on request to the claimant or representative. A letter of authorization will always be used to arrange for examination of an employee and/or review of the case file by a specialist.
d. Field Nurses. OWCP may also utilize the services of a Field Nurse (FN) in facilitating and coordinating medical care for the injured employee. See FECA PM 2-0811 for more information on Field Nurse services.
Back to Chapter 3-0300 Table of Contents
3. Form CA-16, Authorization for Examination and/or Treatment. Form CA-16 is the vehicle by which the employing agency authorizes initial examination and/or medical treatment at OWCP expense. It is used to refer an employee who sustains a traumatic injury to a local physician or hospital of the employee's choice. The employer may not authorize examination or medical treatment in any case that OWCP has disallowed.
a. Traumatic Injury.
(1) Period of Authorization. Form CA-16 authorizes treatment for 60 days from the date of injury, unless OWCP terminates the authorization sooner. The Office has a contractual obligation to pay for medical services and instructs physicians to contact the district office for extension of that period. K.D., Docket No. 11-16 (issued August 16, 2011) [While the chiropractor's report was insufficient to establish that the May 5, 2010 MVA caused or aggravated a diagnosed medical condition, the Form CA-16 authorization from the employing establishment created a contractual obligation to pay for the cost of necessary medical treatment until OWCP terminated the authorization of medical treatment on June 21, 2010.]
(2) Effect of Adjudication. Once a case is accepted, the period of authorization is automatically extended to cover necessary services for the accepted condition, and additional authorization is not necessary unless requested by a provider in a specific case. If a case is denied, however, authorization for further treatment must be revoked even though 60 days have not elapsed.
(3) Emergency Circumstances. Form CA-16 may be used to authorize treatment in cases of a doubtful nature, and in emergencies or unusual circumstances by completing Form CA-16 and checking block 6B of the form.
OWCP may approve payment for medical expenses incurred even if Form CA-16 has not been issued and the claim is subsequently denied. Payment in situations meeting these criteria must be determined on a case-by-case basis (see Val D. Wynn, Docket No. 88-1813, issued March 10, 1989). D.P., Docket No. 11-50 (issued October 26, 2011)
(ECAB held that although there was insufficient rationalized medical evidence to establish appellant's claim of injury, OWCP failed to consider whether emergency or otherwise unusual circumstances were present such that reimbursement of medical expenses would be appropriate even though a CA-16 had not been issued in this case.)
For example, if an employee sustains an injury due to a car accident while on travel and a CA-16 is not issued, OWCP should consider whether payment of expenses is appropriate.
b. Occupational Disease. Form CA-16 should not ordinarily be used in occupational disease claims. The employing agency must contact OWCP for instructions on providing treatment in cases where an occupational disease is claimed. Only in exceptional circumstances will OWCP permit the employing agency to issue Form CA-16 for examination and/or treatment in these circumstances.
c. Excluded Providers. If Form CA-16 is inadvertently released to an excluded provider, the bills should be paid, but a letter rescinding the authorization should be released immediately to the claimant and provider.
Back to Chapter 3-0300 Table of Contents
4. Prohibited Authorizations. No authorization for medical care may be given unless a notice of injury or occupational disease has been or is about to be filed (that is, a notice of injury has been completed and is in possession of the employing agency). The following kinds of authorization are prohibited:
a. Excluded Providers. Although an employee has the right to choose the initial treating physician, no authorization may be given for examination and/or treatment by an excluded physician. For further information regarding excluded providers, see FECA PM 3-0800.
b. Issuance to Oneself. An injured employee does not have the authority to issue a CA-16 on his or her own behalf. For example, if a postmaster sustains an injury, it is expected that authorization will be secured from the regional office. In an emergency, the services of the nearest physician or hospital may be utilized without prior authorization, with the understanding that the employee will contact the employing agency at the earliest possible time for authorization or instructions.
c. Issuance to Minors. OWCP does not consider any person under the age of 18 to be emancipated. Therefore, permission from the parent or guardian will be needed to authorize treatment of any claimant under 18. If the parent or guardian is not immediately available for signed consent, it may be necessary to arrange for a witnessed telephone call to obtain consent. The information obtained should be documented in a call or memorandum for the file.
d. Issuance to Certain Employees Prior to Separation. Certain groups of claimants are entitled to FECA coverage by virtue of special legislation. They include Peace Corps and VISTA volunteers, as well as Job Corps enrollees. While members of these groups are entitled to medical care for accepted injuries at OWCP expense, authorization for treatment may not be granted until the volunteer or enrollee is separated from the program.
e. Advance or Blanket Authorization. An authorization for treatment at some future time, or as the need arises, is not to be issued. When such authorization is requested, the employee should be advised to contact OWCP and/or its designated billing agent as the need for treatment arises.
f. Fitness-For-Duty Examinations. The FECA statute does not provide for examination to determine the "fitness-for-duty" status of an employee. Such an examination is a function of the employing agency. See generally 20 C.F.R. §10.324.
g. Exposure to Disease. The law does not provide for routine examination of an employee who has been exposed to a co-worker with an infectious disease or to hazards of the workplace. Unless there is reasonable proof that a disease or illness has been sustained by the employee, such examinations are the responsibility of the employing agency (see PM Chapter 3-0400). The decision to authorize examination at OWCP expense in these cases must be made by OWCP. See generally 20 C.F.R. §10.303.
Back to Chapter 3-0300 Table of Contents
5. Medical Facilities Where Care May Be Authorized. The FECA at 5 U.S.C. 8103 permits the employee an initial choice of physician. Examination and treatment may be given in the following settings:
a. Emergency Medical Facility. Emergency medical care by private physicians, clinics or hospitals may be authorized if such care is warranted. The employee may seek continuing medical care from the physician who provided the initial treatment or select another local physician.
b. Employing Agency Health Units. These facilities are equipped to provide immediate assistance and/or to refer employees to local physicians or emergency care facilities. When indicated, rescue squads or similarly trained and equipped units may be used to move injured persons.
c. Physician's Office. Ordinarily, the physician selected should be located within a reasonable distance of the employee's home or place of employment, and travel should be undertaken by the shortest route, and, if practical, by public conveyance. If the medical evidence shows that the employee is unable to use these means of transportation, OWCP may authorize travel by taxi or special conveyance. A reasonable distance of travel up to a roundtrip distance of 100 miles is permitted. See 20 C.F.R. §10.315.
d. Hospital. The attending physician may arrange for care in a local hospital. A private room may be authorized only if the condition is such that the attending physician believes it is medically necessary and the DMA concurs. If a private room is used because of the claimant's personal preference, he or she will be required to pay the difference in cost.
e. Federal Medical Facilities. The medical facilities of the Army, Navy, Air Force, and Department of Veterans' Affairs may be used to provide treatment if practicable. If necessary, arrangements can be made on a case-by-case basis with the director of the hospital or clinic (such arrangements should be documented on a CA-110, Report of Call, or in a memorandum for the file). Use of Federal facilities may not be required to the exclusion of the claimant's choice of physician.
Back to Chapter 3-0300 Table of Contents
6. Transfer or Termination of Authorization for Medical Care. Any transfer of medical care should be accomplished with due regard for professional ethics and courtesy. No transfer or termination of treatment should be made unless it is in the best interest of the claimant and the government. The following guidelines should be observed:
a. Request by Official Superior. The official superior of an injured employee does not have authority to transfer medical care from one physician to another. If adequate medical care is not available locally, or the employer feels transfer of medical care is advisable for other reasons, the official superior should contact OWCP for instructions.
b. Request by Attending Physician. If the attending physician asks to be relieved of responsibility in a case, the request will be granted. The physician should be asked to provide his or her reasons for the request, report the patient's condition at the time, and state any further medical recommendations.
c. Request by Employee. Employees who want to change attending physicians must explain their reasons in writing, and the CE must review all such requests.
(1) The CE may approve a change on his or her own authority when: the original treating physician refers the claimant to another physician for further treatment; the claimant wants to change from the care of a general practitioner to that of a specialist in the appropriate field, or from the care of one specialist to another in the appropriate field; or the claimant moves beyond 50 miles from the original physician (since OWCP has determined that a reasonable distance of travel is up to a roundtrip distance of 100 miles).
(2) The CE must use discretion in cases where other reasons are presented:
(a) Denial solely on the basis that the claimant did not seek approval of the change before consulting another physician is improper (see Cybil L. Slade, 40 ECAB 1029). Rather, the CE must examine the request to determine whether the treatment was reasonable and necessary. (See Arron G. Marston, Docket No. 88-1716, issued March 22, 1989). This assessment may require referral of the case to the DMA.
(b) A request to change from the care of a specialist to the care of a non-specialist may not be denied without considering whether the treatment provided by the new physician is reasonable and necessary. However, unless the issue has arisen because care by a specialist is not available, the case should usually be referred for opinion from the DMA.
(c) Likewise, where the claimant wishes to change from the care of a medical doctor to that of a chiropractor, the CE should consult the DMA to determine whether the services of the chiropractor constitutes medical treatment under the Act and, if so, whether it is reasonable and necessary (see Elizabeth J. Davis-Wright, 39 ECAB 1232).
(3) Cases involving complex medical issues should be referred for opinion from the DMA.
(4) A second opinion examination may be in order if a claimant requests transfer to another physician at a time when the treating physician is recommending return to employment. If a second opinion is necessary to address issues involving continuing medical care, the selected physician may not become the treating physician.
d. Questions about Treatment. If the employee is under the care of a qualified physician and a question arises concerning the physician's medical management of the case (for instance, the prolonged use of therapeutic measures or the use of measures of questionable value), it is proper to request the physician's comments, and the DMA may request discussion of the medical problem involved. A second opinion may also be necessary.
e. Request for Consultation. OWCP may seek consultation services with experts in specialized fields, either to provide the attending physician with guidelines or to assist in determining a future course of action with regard to medical care.
f. Transfer of Care. When it is determined that a transfer of medical care is needed, the claimant and the previous attending physician (if not already aware) must be notified in writing regarding the change so that the physician may close his or her file and submit a final bill and report. A suitable explanation should also be furnished to the attending physician if he/she was not involved in the transfer of care request. If appropriate, the physician should be assured that OWCP's action is not intended as a criticism of his or her management of the case or professional ability and judgment. The claimant, as well as the physician, should be advised that authorization for treatment is being terminated.
g. Exclusion of Provider. As noted above, OWCP must terminate authorization for treatment with excluded providers. Both the physician and the claimant should be advised immediately that further medical treatment is not authorized, and the claimant should be advised to select another treating physician. The claimant may continue to receive treatment from the excluded provider at his or her own expense. Exclusion of providers is discussed in Chapter 3-0800.
Back to Chapter 3-0300 Table of Contents
|
Paragraph and Subject |
Date |
Trans. No. |
|---|---|---|
|
Table of Contents |
06/00 |
00-07 |
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
|
10/95 |
96-04 |
|
|
09/95 |
95-39 |
|
10/90 |
91-02 |
|
|
|
04/92 |
92-17 |
|
04/92 |
92-17 |
|
|
|
04/93 |
93-24 |
|
06/00 |
00-07 |
|
|
|
04/92 |
92-17 |
|
04/92 |
92-17 |
|
|
04/92 |
92-17 |
|
|
|
09/95 |
95-39 |
|
04/92 |
92-17 |
|
|
04/92 |
92-17 |
1. Purpose. Many forms of treatment, including diagnostic procedures, may be authorized by OWCP when prescribed by the attending physician. Similarly, many supplies may be provided at the request of the attending physician or claimant. This chapter describes the circumstances under which such treatments and supplies may be authorized.
Back to Chapter 3-0400 Table of Contents
2. Statutory Authority. While OWCP generally does not have authority to require an injured employee to undergo treatment against his or her will, it is assumed that employees will seek appropriate treatment to restore health and lessen the severity of impairment. Services and supplies which meet the statutory criteria of being "likely to cure, give relief, reduce the degree or the period of disability, or aid in lessening the amount of the monthly compensation" (5 U.S.C. 8103(a)) may be approved.
Back to Chapter 3-0400 Table of Contents
3. Supplies and Appliances. Specific supplies and appliances and the conditions under which they may be authorized are as follows:
a. Prescription and Non-Prescription Drugs. In general, drugs and medications which are necessary to treat an injury or occupational disease may be purchased at OWCP expense on the recommendation of the attending physician. These include prescription as well as non-prescription medications. Cases requiring prolonged use of narcotic preparations, tranquilizers, or medicinal alcohol must be referred to the DMA for consideration of continued authorization.
b. Home Medical Supplies and Appliances. Items such as rubbing alcohol, thermometers, sun lamps, heating pads, analgesics, antacids, etc., will not be furnished at OWCP expense unless prescribed by the attending physician and justified medically. Accepted conditions which may warrant furnishing such items include such conditions as paraplegia, quadriplegia, coma, and chronic ulcers. The Claims Examiner (CE) does not need to obtain approval for the use of these items but may need to consult the District Medical Adviser (DMA) to determine the frequency with which they are needed.
c. Durable Medical Equipment.
(1) Orthopedic Mattresses or Hospital Beds. These appliances may be authorized when prescribed by the attending physician to relieve orthopedic or other medical conditions, but less costly alternatives such as a bed board should be considered first whenever possible.
(2) Motorized Wheelchairs. The purchase or rental of a motorized wheelchair may be authorized when the condition necessitating it is considered to be permanent. Recommendations for this equipment shall be referred to the DMA for advice regarding authorization.
(3) Other Equipment. Such items as traction apparatus and walkers for home use may be authorized upon the recommendation of the attending physician if their use is warranted by the accepted condition.
d. Prosthetic Devices and Other Personal Appliances.
(1) Glasses and Contact Lenses. Glasses and contact lenses for the correction of refractive error will be furnished for a condition accepted as work-related, and subsequent repair or replacement will be authorized as necessary.
(a) When OWCP accepts a case for loss of vision or loss of an eye, the purchase of glasses or contact lenses will be authorized for correction of refractive error in the uninjured eye.
(b) Prescription sunglasses will be authorized when recommended by a qualified physician in cases following cataract surgery. When recommended for another approved condition, the opinion of the DMA should be obtained prior to acting on the recommendation.
(c) Intraocular implant lenses are imbedded in the eye to correct vision in some older patients when cataract surgery is performed. They may be authorized on recommendation of the attending ophthalmologist.
(2) Hearing Aids. Hearing aids will be authorized when hearing loss has resulted from an accepted injury or disease if the attending physician so recommends. Trial or rental periods should be encouraged as many persons do not find their use satisfactory. Maintenance of hearing aids provided by OWCP, including batteries, repairs, and replacements, may be authorized as needed.
(3) Orthopedic Shoes. If an accepted injury to the foot modifies its structure so that the employee cannot be fitted with ordinary shoes, specially constructed ready-to-wear or custom built shoes may be furnished upon the recommendation of the attending physician. If such shoes will be required permanently, the purchase of two pairs may be authorized. Alterations to stock shoes usually worn by the claimant will also be authorized if needed.
(4) Artificial Limbs and Braces. These devices may be authorized as recommended by the attending physician.
(5) Non-medical Equipment. Items such as waterbeds, saunas, weight-lifting sets, exercise bicycles, etc., may be authorized only if recommended by the attending physician and if OWCP finds that the item is likely to cure, give relief, reduce the degree or the period of disability, or aid in lessening the amount of monthly compensation. Procedures for developing and adjudicating requests for such equipment are provided in PM 2-810.15.
(6) House and Vehicle Modifications. Procedures for developing requests for modification of houses and vehicles due to the accepted condition are provided in PM Chapter 2-1800. Requests for items such as home wheelchair ramps, special automobile attachments, and window air conditioning equipment should be handled in accordance with paragraph (5) above.
Back to Chapter 3-0400 Table of Contents
4. Obtaining Appliances and Arranging for Repairs. Appliances may be either personal or non-personal in nature.
a. Personal Appliances. Devices which are specifically fitted to and worn by the claimant, such as back braces, eyeglasses, and artificial eyes are considered personal rather than government property. Upon the recommendation of the attending physician, such appliances may be repaired or replaced without advance approval when the estimated cost is less than $500. Repairs or replacements costing more than this amount should be approved in advance by the DMA if possible. The attending physician should check the repaired or replaced item to ensure a proper fit.
b. Non-personal Appliances. Prior to authorizing any item of a non-personal nature, the cost of purchase should be compared to the cost of renting, taking into consideration the prognosis and the estimated duration of need. Generally, the less expensive method will be used. When the item is rented, the Medical Management Assistant (MMA) will place a six-month call-up to assess whether the item is still needed for the accepted condition and if rental is still less costly than purchase.
A purchased item which can be salvaged when no longer required by the employee will be considered government property if its retail value is more than $5000. Such items as hospital beds and wheelchairs fall into this category, and the employee must be notified in writing at the time of purchase that the property may be recovered by the government at a later date. When the item is no longer needed, the MMA will contact at least one nearby Federal medical facility and offer it for pickup at no expense to OWCP. If the facility does not wish to acquire the item, the MMA will notify the regional office of the General Services Administration that the item is available.
c. Repair and Replacement.
(1) The definition of "injury" at 20 C.F.R. 10.5(a)14 includes:
damage to or destruction of medical braces, artificial limbs, and other prosthetic devices which shall be replaced or repaired; except that eyeglasses and hearing aids shall not be replaced, repaired, or otherwise compensated for, unless the damage or destruction is incident to a personal injury requiring medical services.
(2) Medical braces, artificial limbs, and other prosthetic devices covered under this provision can be repaired or replaced on a one-time basis in the absence of any other medical condition resulting from a work-related incident. OWCP can authorize repair or replacement of property, such as eyeglasses, hearing aids, and artificial teeth, which is damaged or destroyed while in the performance of duty only when the damage or destruction is incident to a personal injury requiring medical services, or when an accepted condition requires change in a prosthesis used at the time of injury.
(3) When OWCP cannot authorize repair or replacement, the CE should advise the claimant that under 31 U.S.C. 240-243, Federal establishments may settle and pay claims against the United States by its civilian employees for damage to, or loss of, personal property incident to employment. The CE should also advise the claimant to contact his or her supervisor to determine whether a claim may be made under this statute.
Back to Chapter 3-0400 Table of Contents
5. Medical Services. Services which meet the statutory criteria of being "likely to cure, give relief, reduce the degree or the period of disability, or aid in lessening the amount of the monthly compensation" may be authorized. The circumstances under which various kinds of services may be authorized are described below. Any denial of services requested by the claimant or attending physician must address these criteria.
a. Emergency Medical Facility. Emergency medical care by private physicians, clinics or hospitals may be authorized if such care is warranted.
b. Hospital. The attending physician may arrange for care in a local hospital. A private room may be authorized only if the condition is such that the attending physician believes it is medically necessary and the District Medical Advisor (DMA) concurs. If a private room is used because of the claimant's personal preference, he or she will be required to pay the difference in cost. Also, such personal items as television and telephone service must remain the claimant's responsibility.
(1) Surgery. In an elective or non-emergency situation, the file must be reviewed by a specialist prior to authorizing surgery for a back condition, an organ transplant or a destructive procedure. A second opinion examination may be obtained at Office expense prior to authorization for surgery or any invasive procedure (see Chapter 3-500 concerning second opinion requests). In-house review by the consultant should occur within 21 days of receipt of the request for surgery, and any second opinion examination required should be accomplished within 40 days. Plastic surgery for cosmetic reasons may not be authorized unless it is performed for a disfigurement of the face, head or neck which has been accepted by the Office.
(2) Organ Transplants. Organ transplants, except for those which are experimental or not generally accepted by the medical community, may be approved upon the attending physician's recommendation and OWCP's approval consistent with its second opinion procedures. Ancillary treatment such as immunosuppression is also considered compensable.
An organ donor is not considered an "employee" within the meaning of the FECA and is not entitled to compensation for wage loss or permanent impairment, nor is a donor entitled to benefits for any complications resulting from the transplant. Only those medical and related expenses of the donor which are necessary to secure treatment for the employee are allowable.
(3) Destructive and Questionable Measures. Such procedures as rhizotomy, injection treatment for varicose veins, chordotomy, neurectomy, etc., will not normally be authorized solely because of chronicity of a condition. They may be authorized as a measure of last resort, after adequate consultation with specialists in the appropriate field of medicine. Medical or surgical treatment of a questionable nature will not be authorized without adequate consultations. Second opinion examinations and OWCP approval are required for any such procedure.
(4) Substance Abuse Treatment. Where recommended by the treating physician, the Office may approve a one-time inpatient substance abuse treatment program up to 28 days in length. Such a program may be approved even if the Office has not accepted substance abuse as related to employment in cases where the abuse is hindering the claimant from participating in a rehabilitation program or securing employment. The treatment facility should be located within 25 miles of the claimant's home wherever possible, and a cost comparison between comparable facilities should be made before care is authorized. Any request for a subsequent course of inpatient substance abuse treatment should be forwarded to the National Office for consideration.
Outpatient treatment may be recommended by itself or as a follow-up measure to inpatient care. Such treatment may be authorized when recommended by the attending physician, as may medications prescribed to alleviate the effects of addiction (e.g., Antabuse). Likewise, counseling in a group setting may be undertaken at OWCP expense.
c. Outpatient or Ambulatory Services. In addition to treatment in the physician's office, the following may be authorized:
(1) Nursing Services. See paragraph 6 below.
(2) Physical Therapy. For any orthopedic or neurological condition, physical therapy for a period of 90 days may be authorized if prescribed by the attending physician. Any therapy in excess of 90 days requires additional medical justification. The time limitation does not apply to cases involving brain and spinal cord injuries, extensive second and third degree burns and other conditions which have rendered the claimant bedridden. (See FECA PM 2-810.16 for a detailed discussion of authorization of physical therapy.) Work hardening programs may also be considered on recommendation of the treating physician.
(3) Occupational and Speech Therapy. These services may be authorized when recommended by the attending physician for reasonable periods if improvement or relief of distress is likely to result. Long term therapy without prospect of improvement shall not be authorized. Recommendation for such therapy is usually referred to the DMA for consideration. Occupational or speech therapy may be authorized when performed in recognized facilities or when rendered by private providers as long as it is prescribed by the treating physician and he or she monitors the results.
(4) Lip-Reading Services. On recommendation of the attending physician, the DMA may approve lip reading services if they would likely reduce the extent of disability and aid in rehabilitation.
(5) Pain Clinics. The DMA may authorize pain clinic treatment only if it is appropriate for the accepted condition and the clinic in question is reputable. Whenever possible clinics connected with universities or other teaching institutions should be used.
(6) Palliative Treatment. The DMA may authorize such treatment for prolonged or terminal conditions when the need is adequately supported by consultants. The therapy may consist of surgical procedures (rhizotomy), nerve blocks, large doses of pain medications, and the services of pain clinics or hospices.
(7) Specific Treatments. In addition to the routine diagnostic and therapeutic services provided in an institution or professional office, specific forms of treatment may be authorized as follows:
(a) Acupuncture. Acupuncture may be authorized when recommended by the attending physician to provide relief. Such treatment shall be supervised by the recommending physician, who shall submit periodic reports to show progress or any relief of the symptoms. If the treatment continues beyond six months and/or the results are questionable, the DMA should be asked for an opinion as to whether the treatment should continue.
(b) Chymopapaine Treatment. Serious side effects have been reported from the injection of chymopapaine. Therefore, any request for this form of treatment must be justified by the attending physician and reviewed by the DMA.
(c) Hernia Treatment. Surgery is the usual treatment authorized for a hernia. If surgery is refused or medically contraindicated, the fitting of a truss may be authorized if recommended by an examining physician. Injection treatments are now very rarely used and any such request should be referred to the DMA for opinion.
(d) Substance Abuse Treatment. Such treatment may be authorized on the basis of the attending physician's recommendation. Such a program may be approved even if the Office has not accepted substance abuse as related to employment in cases where the abuse is hindering the claimant from participating in a rehabilitation program or securing employment.
d. Dental Services. The law provides for repair or replacement of injured natural and fixed artificial teeth. Except in dental emergencies, prior approval of OWCP shall be obtained for dental repair or replacement. Before approving dental repair or replacement, an examination including x-ray and prophylaxis should usually be authorized and an estimate of the cost of the proposed dental work must be obtained.
Back to Chapter 3-0400 Table of Contents
6. Nursing Services. OWCP uses the services of in-house Staff Nurses and contract Field Nurses to coordinate claimants' medical care and aid them in returning to work. The work of the Staff Nurses is discussed briefly in PM 3-200 and more thoroughly in PM 3-201. The following guidelines pertain to requests for clinical nursing services:
a. Licensed or Practical Nurse. The services of these nurses may be authorized when recommended by the attending physician for therapeutic services in the home. The services of a nurse may not be authorized to perform housekeeping duties, however.
(1) Nursing Plans. Nursing agencies routinely develop nursing care plans for home care which are based on the treating physician's instructions. A copy of the plans should be obtained to verify that the nursing care proposed is related to the accepted condition. Absent such plans, the following questions may be posed to the attending physician:
(a) What are the chronic sequelae of the work-related injury and what form of treatment do they require?
(b) Are there acute and/or recurrent complications of these sequelae? How frequently do they appear? What form of treatment do they require?
(c) Has the claimant required hospitalization for the treatment of any of the chronic sequelae and/or complications? How frequently?
(d) What is the anticipated duration of nursing services?
(2) Special Nurses. The services of special nurses may be authorized when the attending physician certifies that such services are necessary due to the severity of the claimant's condition. In questionable cases, the case file should be referred to the DMA for recommendation. A care plan should be obtained and the approval period tailored to the needs of the claimant in accordance with the physician's recommendation.
b. Services of Relatives. The attending physician must approve the qualifications of a relative acting as a nurse to provide the necessary services.
c. Extended Care Facilities. Care in a convalescent home, skilled nursing facility or hospice may be authorized when the employee does not need acute care but does require services difficult or impossible to arrange in the home setting. The recommendation of the attending physician is required in this situation. OWCP will pay the rates for standard accommodations according to the requirements of the medical condition. The claimant should remain under continuing medical supervision of a physician, who may be asked to justify the continuing need for institutional care every three to six months according to the severity of the claimant's medical condition.
Back to Chapter 3-0400 Table of Contents
7. Other Modes of Treatment.
a. Preventive (Prophylactic) Treatment. The FECA does not authorize provision of preventive measures such as vaccines and inoculations, and in general, preventive treatment is a responsibility of the employing agency under the provisions of 5 U.S.C. 7901. However, preventive care can be authorized by OWCP for the following:
(1) Complications of preventive measures which are provided or sponsored by the agency, such as adverse reaction to prophylactic immunization.
(2) An injury involving actual or probable exposure to a known contaminant, thereby requiring disease-specific measures against infection. Included among such treatments would be tetanus antitoxin or booster toxoid injections for puncture wounds; administration of rabies vaccine where a bite from a rabid animal, or one whose status was unknown, is involved; or AZT where exposure to HIV virus has occurred.
(3) Periodic examination of the uninjured eye may be authorized where injury to the other eye has resulted in loss of vision, so that possible sympathetic involvement of the uninjured eye may be detected at an early stage. The frequency of these examinations should be determined on the basis of the attending physician's recommendations. If sympathetic involvement of the uninjured eye is found, appropriate medical and surgical treatment for this condition will be authorized.
(4) Conversion of tuberculin reaction from negative to positive. In this situation INH therapy may be authorized. Treatment is limited to the injured employee and cannot be extended to others who may, for example, have been exposed to an infectious agent by the employee.
b. Adjunct and Ancillary Treatment. Upon the recommendation of the attending physician, treatment may be authorized for a concurrent ailment if it appears that such treatment is closely related to the treatment of an injury and would hasten the cure of the accepted condition(s). Requests for such treatments may include such regimes as weight loss programs for claimants with chronic back conditions as well as more traditional therapies such as treatment of concurrent diabetes in claimants with eye or foot conditions. The DMA must review all such requests prior to authorization.
c. Experimental Treatment and Clinical Research. All requests for authorization of the following kinds of treatment or research should be referred to the OWCP Medical Director following appropriate development:
(1) Experimental diagnostic and treatment modalities or those which are not generally accepted. Experimental treatment modalities will be considered if the accepted condition is life-threatening (e.g., cancer or AIDS); established therapy has been tried to no avail; and a significant body of data supports the view that the experimental procedure is indeed beneficial;
(2) Participation in a research protocol;
(3) Administration of questionnaires, particularly of a sociological or psychological nature.
Such requests should not be approved or denied without advice from the National Office.
Back to Chapter 3-0400 Table of Contents
8. Non-medical Services.
a. Health Club/Spa Membership. Membership in a health club or exercise facility, or treatment at a spa, may be authorized when recommended by the attending physician as likely to cure or give relief. Only the facilities required should be authorized (for example, if swimming is prescribed, the approval should not include use of exercise equipment as well) and the least expensive facility in the area should be used. Procedures for developing and adjudicating requests for health club/spa membership are provided in PM Chapter 2-810.15.
b. Seeing Eye and Hearing Dogs. The OWCP may pay for seeing eye and hearing dogs, as well as for their training and maintenance costs, on prescription of the attending physician if this service is required because of blindness in both eyes or severe deafness (at least 80 percent binaural loss) resulting from factors of the employment.
c. Change in Locality. Where a physician recommends that an injured employee visit or move to another climate to alleviate symptoms of the employment-related condition, the expenses incurred may be authorized if OWCP finds that such a move is likely to cure, give relief, reduce the degree or period of disability, or aid in lessening the amount of monthly compensation. After developing the evidence, the CE should refer the case file to the DMA for opinion concerning the advisability of such a move.
Back to Chapter 3-0400 Table of Contents
9. Injury or Death While Obtaining Medical Care.
a. Benefits Payable. When an employee is injured while traveling to or obtaining authorized medical care or examination, he or she is entitled to medical benefits just as if the injury had occurred in the performance of duty. If an injured employee dies away from home while receiving medical examination or treatment, the body may be embalmed and transported in a hermetically sealed casket to the employee's home at OWCP expense even if death did not result from an accepted injury. If death resulted from a condition unrelated or questionably related to the accepted condition, authorization for services should include a request for postmortem examination.
b. Pathological and Postmortem Examinations. The DMA may authorize pathological examination of removed tissue at OWCP expense if such examination is necessary to determine the merits of a claim that has been or will be filed. If a postmortem examination has not been ordered by the coroner or local medical examiner, permission for such an examination must be requested in accordance with the appropriate state law.
c. Autopsy. If an autopsy is authorized, the DMA should specify that it be conducted by a pathologist or another physician fully qualified to perform such services and that a complete autopsy protocol must be submitted prior to payment of the bill. Authorization for this procedure may be given by telephone, followed by written confirmation or by telegram (where the medical examiner is overseas). See PM Chapter 2-700 for additional information concerning autopsies.
Back to Chapter 3-0400 Table of Contents
10. Transportation and Expenses. OWCP will reimburse the cost of transportation needed for treatment or examination of the claimant for the accepted injury, unless transportation is furnished by the government. The transportation costs may include the services of an accompanying nurse or attendant if required (see paragraph 6a(4) above). Incidental expenses may also be reimbursed whether or not transportation is furnished by the Government, but OWCP cannot advance funds to defray travel and incidental expenses except as noted below.
a. Mode of Travel. Travel should be undertaken by the shortest route, and if practical, by public conveyance such as bus or subway. If the medical evidence shows that the employee is unable to use these means of transportation, the CE may authorize travel by taxi or special conveyance.
Transportation by ambulance may also be authorized if required, and if travel by air ambulance is indicated, or air ambulance is found to be more economical and expeditious than ordinary commercial air transportation, approval may be granted for this service. In all such instances the DMA will be consulted for advice, by telephone if indicated.
b. Transportation Expenses. Standard Form 1012 and Form CA-1077 shall be sent to the injured employee whenever examination and/or treatment is authorized. They are used to claim reimbursement for travel expenses when the government does not furnish transportation. When the employee must travel to secure authorized examination and/or treatment and the travel will cost more than one hundred dollars by public transportation, a Government Transportation Request (GTR), Standard Forms 1169 and 1169a, may be issued. The claimant should be instructed to return a GTR which is not used so it can be canceled.
c. Accompaniment While Traveling. If the employee requires a nurse or an attendant to accompany him or her in securing examination and/or treatment, this service and associated transportation and incidental costs may be authorized. Unless a need for other arrangements is demonstrated, he or she should be instructed to make the return trip as soon as possible so that no unnecessary expense will be incurred.
d. Incidental Expenses. Charges for child care, pet care, and home security may be paid when incurred in the course of securing medical services and supplies. In each case, the record must contain a memorandum discussing the need for the incidental expenditure and the reasonableness of the amount claimed.
(1) Necessity and Reasonableness. Incidental expenses shall be paid to the extent that they are necessary and reasonable. For example, in a household consisting of the claimant, a child, and a semi-invalid parent where the claimant must pay for care of the child and parent while hospitalized, reasonable family care expenses would be paid. Should additional expenses be claimed, such as a kennel for the family dog, reasonable kennel charges would be paid only if it were determined that other arrangements could not be made, such as pet care by the person staying with the family.
(2) Timing of Expense. Incidental expenses are allowable only when incurred in the course of securing medical services and supplies. Therefore, it is necessary to distinguish between expenses connected with securing treatment and those incurred following treatment.
Expenses in the latter category, such as housekeeping costs while the claimant convalesces at home, are not payable because they are not required to obtain medical services.
Back to Chapter 3-0400 Table of Contents
|
Paragraph and Subject |
Date |
Trans. No. |
|---|---|---|
|
Table of Contents |
12/12 |
13-04 |
|
7/11 |
11-06 |
|
|
7/11 |
11-06 |
|
|
7/11 |
11-06 |
|
|
7/11 |
11-06 |
|
|
6/15 |
15-02 |
|
|
7/11 |
11-06 |
|
|
5/13 |
13-08 |
|
|
12/12 |
13-04 |
|
|
7/11 |
11-06 |
|
|
7/11 |
11-06 |
1. Purpose. This chapter describes the two kinds of OWCP directed medical examinations, second opinion and impartial referee medical examinations, and the steps involved in scheduling these examinations.
Other Federal Employees' Compensation Act (FECA) Procedure Manual chapters also have relevant guidance pertaining to medical examinations and should be consulted.
Chapter 2-0810, Developing and Evaluating Medical Evidence, discusses the Claims Examiner's (CE's) function in evaluating medical evidence and authorizing treatment. It has specific sections devoted to the decision-making process for obtaining second opinion and referee examinations.
Chapter 3-0300, Authorizing Examination and Treatment, discusses the circumstances under which OWCP or, in some instances, the employing agency may authorize medical services and treatment for injured claimants.
Chapter 3-0600, Requirements for Medical Reports, outlines the information that should be included in all medical reports.
Back to Chapter 3-0500 Table of Contents
2. Statutory Requirements. The authority to schedule second opinion and referee examinations is specifically noted in the FECA in §8123, which states:
An employee shall submit to examination by a medical officer of the United States, or by a physician designated or approved by the Secretary of Labor, after the injury and as frequently and at the times and places as may be reasonably required. The employee may have a physician designated and paid by him present to participate in the examination. If there is disagreement between the physician making the examination for the United States and the physician of the employee, the Secretary shall appoint a third physician who shall make an examination.
Back to Chapter 3-0500 Table of Contents
3. Second Opinion Examinations. The attending physician (AP) is the primary source of medical evidence in most cases, and the AP is expected to provide a rationalized medical opinion based on a complete medical and factual background in order to resolve any pending issues in a case. In certain circumstances, such as where the AP's report does not meet the needs of the OWCP, OWCP may schedule a second opinion examination (SECOP).
a. Determining the Need for Examination. The decision to refer a case for a second opinion examination rests with the CE, though such an exam may be recommended by a Field Nurse (FN) or District Medical Advisor (DMA), or requested by the employing agency. A complete discussion of when a CE should refer a case for a second opinion examination is found in PM 2-0810-9 and 2-810-10.
Also, OWCP may send a case file for second opinion review where actual examination is not needed, or where the employee is deceased.
b. Selection of SECOP Physician.
(1) Physicians selected to perform second opinion examinations should be administratively qualified in the appropriate branch of medicine.
(a) Where an emotional condition is the only work-related condition known to be present, a referral can be made to a psychiatrist or a clinical psychologist (as long as the file contains no indication that medication for a psychological condition is being used). Referral to a clinical psychologist may be made even if the attending physician is a psychiatrist, but not where psychogenic overlay is felt to be present, as these cases presuppose a connection between the psychological condition and its physical manifestation which can best be addressed by a psychiatrist.
(b) If the issue for determination is the causal relationship between a workplace injury/factor and a claimed condition or a claimant's ability to perform the date of injury position or some other type of modified work, a referral can be made to a specialist in occupational medicine, even if the attending physician is an orthopedist, neurologist or some other specialty. As a sub-specialty under the Board of Preventive Medicine, occupational medicine physicians are specialists in the field of workplace injuries and illnesses and their causal associations. They also specialize in assessing fitness for duty relevant to the employee's work environment.
(2) Second opinion examinations are generally conducted by a physician selected by a medical referral group that has contracted with OWCP to provide second opinion medical referrals. The method for selecting second opinion physicians is more flexible, since a strict rotation of physicians is not required for this type of examination.
(3) If the medical referral group is unable to schedule the necessary appointment in accordance with the needs of OWCP, OWCP can use the Medical Management application for this purpose (see paragraph 5 below).
c. Information Sent to Second Opinion Physician. The physician should be provided with the following:
(1) A statement of accepted facts (SOAF);
(2) A list of pertinent questions or issues to be addressed;
(3) Copies of medical records from the case file based on the age of the case and/or the nature of the referral as follows:
(a) For unadjudicated case referrals and all referrals for medical management, disability management or surgery:
(i) All operative reports regardless of age;
(ii) All diagnostic tests regardless of age; and
(iii) All medical records from any qualified physician as defined in 5 U.S.C. 8101(2) authored within three years of the date of the second opinion referral.
(b) For schedule award referrals:
(i) All operative reports regardless of age;
(ii) All diagnostic tests regardless of age;
(iii) All medical records from any qualified physician as defined in 5 U.S.C. 8101(2) that address permanent partial impairment and maximum medical improvement; and
(iv) The most current comprehensive medical narrative report from a qualified physician as defined in 5 U.S.C. 8101(2).
If the CE determines in the exercise of his or her judgment that the unique circumstances of a case file require deviation from these requirements in order to assist the physician in rendering a rationalized medical opinion based on an adequate medical background, the CE should document such circumstances and the specific deviations/changes in a Memorandum to the File to be made part of the case record. An example of a situation where inclusion of additional medicals might be appropriate would be in a complex catastrophic case with numerous accepted conditions.
(4) If a medical report has been excluded from the case record, it should be omitted from the medical evidence sent to the second opinion specialist. See PM 2-0810.12.
d. Information Sent to Claimant and the Properly Authorized Designated Representative. Once the appointment has been scheduled, the claimant/representative should be notified. See Donald J. Knight, 47 ECAB 706 (1996) (where ECAB held that OWCP's failure to notify appellant's authorized representative of the referral to a second opinion physician effectively denied appellant's statutory right to have a physician designated and paid by him to be present and participate in the examination pursuant to 5 U.S.C. 8123). This may be done by OWCP, or by the contractor on OWCP's behalf. The claimant and his or her designated representative should be provided with the following information:
(1) The name and address of the physician to whom he or she is being referred, as well as the date and time of the appointment.
(2) The claimant's right, under section 5 U.S.C. 8123 of the FECA, to have a physician paid by him or her present during a second opinion examination. 20 C.F.R. § 10.320; Esther Velasquez, 45 ECAB 249 (1993) (ECAB held that by misinforming the claimant of the purpose of the medical referral, OWCP effectively denied her the right granted by the FECA, and that OWCP was precluded from relying on the resulting medical report "before affording appellant the opportunity to exercise this statutory right.")
Because a claimant has a right under the statute to have such a physician attend a second opinion examination, OWCP may not re-characterize an impartial examination as a second opinion examination in the event it determines there was no conflict in the medical evidence; however, the report need not be excluded and may be considered for its intrinsic value.
(3) A warning that benefits may be suspended pursuant to 5 U.S.C. 8123(d) for failure to report for examination.
(4) Information on how to claim travel expenses.
e. The employee is not entitled to have anyone present at the examination (other than the physician identified in d(2) above), unless the case file or other rationalized medical evidence establishes the need for someone else in the room, or OWCP decides that exceptional circumstances exist. However, where an employee requires an accommodation, such as where a hearing-impaired employee needs an interpreter, the presence of an interpreter or other individual will be allowed. Anthony H. Jackson, 53 ECAB 529 (2002) (ECAB held that a claimant is not entitled to have anyone other than a qualified physician in attendance at a referral medical examination unless OWCP decides that exceptional circumstances exist); Ida L. Townsen, 45 ECAB 750, 757 (1994) (finding that interference by appellant's representative in insisting that he be present for a medical examination constituted obstruction under section 8123 and supported suspension of appellant's benefits).
f. Follow-up Action. Using the SOAF (See FECA PM 2-0809 regarding SOAF requirements) as the framework for his or her opinion, the second opinion physician should provide a report which contains a clinical history, results of the examination, results of any testing performed, and a reasoned opinion in response to the questions posed. A report should be expected within 30 days of the examination.
(1) If no medical report is received within 30 days from the date of appointment, the CE or medical scheduler should inquire as to the status with the medical referral group and/or the second opinion physician. The CE or medical scheduler may also follow up soon after the date of the appointment to verify the claimant's attendance at the appointment. For a complete discussion describing the circumstances under which benefits may be suspended under 5 U.S.C. 8123(d) for failure to attend an appointment, see PM 2-0810-13 Suspension of Benefits.
(2) Upon receipt of the report, the CE should review the report to ensure that the physician has adequately addressed the questions posed.
(a) If clarification or additional information is necessary, the CE should write to the specialist to obtain it, either directly or via the medical referral group, as appropriate.
(b) Upon receipt of any clarifying information, the CE should again review the report to ensure that it is complete and responsive to the questions asked.
Back to Chapter 3-0500 Table of Contents
4. Referee Examinations. Section 8123(a) of the FECA and section 10.321 of the implementing regulations provide for the appointment of a referee physician to examine the claimant and resolve a conflict of medical opinion in a case. This is referred to as an impartial medical examination (IME). Because this method of resolving conflicts is provided in the FECA, the probative value of the referee specialist's report is great and will normally constitute the weight of the medical evidence of record. Y.A., 59 ECAB 701 (2008) (when a case is referred to an impartial medical specialist for the purpose of resolving a conflict in medical opinion, the opinion of such specialist, if sufficiently well rationalized and based on a proper background, must be given special weight).
a. Determining the Need for Examination. A difference in medical opinion sufficient to be considered a conflict occurs when two reports of virtually equal weight and rationale reach opposing conclusions. See James P. Roberts, 31 ECAB 1010 (1980). The CE makes this determination after weighing the opinions. See PM 2-0810-6 for an extended discussion on weighing medical evidence. A complete discussion of when a CE should refer a case for a referee examination is found in PM 2-0810-11. 20 CFR § 10.321(a).
b. Selection of IME Physician. Unlike selection of second opinion examining physicians, selection of referee physicians is made on a strict rotational basis.
(1) OWCP will select a physician who is qualified in the appropriate specialty and who has had no prior connection with the case.
(2) The Employees' Compensation Appeals Board has placed great importance on the appearance as well as the fact of impartiality, and only if the selection procedures which were designed to achieve this result are carefully followed may the selected physician carry the special weight accorded to an "impartial specialist."
In Leonard W. Waggoner, 37 ECAB 676 (1986), ECAB remanded the case because the physician who examined the claimant was an associate of the physician to whom the claimant had been referred. Since the claimant was told to report to one physician but was ultimately examined by another, he had no opportunity to object to the choice of examiner. ECAB did not find that the specialist in this case was in fact biased, or would have been ineligible on any particular ground. Rather, it found that to give special weight to a physician not selected in accordance with procedures would "undermine the appearance of impartiality or would appear to compromise the integrity of the system for selecting impartial specialists." ECAB found that the physician was not entitled to the special weight accorded to a referee specialist because the procedures designed to provide adequate safeguards against any possible appearance of bias were not followed.
(3) Physicians in certain roles may not be chosen to act as referees in specific cases. When a physician is asked to act as a referee specialist, the medical scheduler should inquire as to the nature of any previous association with the claimant or the claimant's employing agency. Physicians who may not be used as referees include:
(a) Those employed by, under contract to, or regularly associated with Federal agencies. See George W. Coast, 36 ECAB 600 (1985) (ECAB held that although there was no direct evidence of record substantiating that the physician was previously connected with the claimant's case, the selection of a physician involved with fitness-for-duty examinations on behalf of the employing establishment undermined the appearance of impartiality).
(b) Physicians previously connected with the claim or the claimant, or physicians in partnership with those already so connected (see Raymond E. Heathcock, 32 ECAB 2004 (1981) (ECAB held that OWCP could not use the report of one physician to resolve a conflict in medical evidence because he was an associate of another physician previously connected with the case, and therefore was not completely independent)).
(c) Physicians who have acted as a medical consultant to OWCP (see John Clement, 35 ECAB 959 (1984)).
Note: The mere fact that a physician has conducted a second opinion examination in connection with the FECA program does not eliminate that physician from serving as an impartial referee physician in another case.
(4) In a case involving only a mental condition where a conflict exists between two psychologists or between a psychologist and a physician who does not specialize in treatment of mental disorders, the referee specialist chosen to resolve the case may be either a psychiatrist or clinical psychologist (as long as the file contains no indication that medication for a psychological condition is being used). In those cases, however, where a conflict has arisen between a psychologist and a psychiatrist or between two psychiatrists, the Office will obtain a referee examination from a psychiatrist. This practice will ensure that the referee physician carries sufficient weight in cases where a medical doctor has been involved in creating the conflict, and should also ensure that the full range of issues is addressed.
(5) In a case involving a physical condition where a conflict exists with regard to the causal relationship between a workplace injury/factor and a claimed condition or a claimant's ability to perform the date of injury position or some other type of modified work, a referee examination may be scheduled with an occupational medicine physician, even if one or both of the physicians with conflicting opinions is not an occupational medicine physician. As a sub-specialty under the Board of Preventive Medicine, occupational medicine physicians are specialists in the field of workplace injuries and illnesses and their causal associations, and they also specialize in assessing fitness for duty relevant to the employee's work environment, they are qualified to provide an opinion on these issues and may be afforded the special weight provided to referee physicians.
(6) The selection of a physician to perform a referee medical examination is done by the district office using the Medical Management application within the Integrated Federal Employees' Compensation System (iFECS). This selection process is described in detail in paragraph 5 of this chapter.
(a) The Medical Management application contains the names of physicians who are Board-certified in certain specialties. The database of Board-certified physicians used for referee examinations contains over 30 specialties, including: cardiovascular disease, dermatology, gastroenterology, internal medicine, neurology, occupational medicine, osteopathy, orthopedic surgery, physical medicine and others.
(b) The services of all available and qualified Board-certified specialists will be used as far as possible to eliminate any inference of bias or partiality. This is accomplished by selecting physicians (in the designated specialty in the appropriate geographic area) in alphabetical order as listed in the roster and repeating the process until the list is exhausted.
(c) A physician can be added to the Medical Management application, and thereby the rotation, by the District Director, or his/her designee after verifying that the physician meets the board-certification requirements for a particular specialty.
(d) A physician may be eliminated from the rotation for the following reasons, which include, but are not limited to: he or she is not willing to perform examinations for OWCP; reports have shown a predictable pattern amounting to bias; he or she chronically submits inadequate reports in the face of acceptable questions; reports are consistently submitted late; or he or she has a signed agreement with OWCP to perform case file reviews.
OWCP may discontinue the use of a physician by properly updating the Medical Management application and citing instances (dates, specific case files, etc.) in which bias or inadequacies are demonstrated. The District Director, or his/her designee, is authorized to suspend or permanently remove a physician.
(e) Excluded providers are disqualified from serving as referee physicians (see Chapter 3-0800).
(f) A physician who is not Board-certified may be used if he or she has special qualifications for performing the examination, but the scheduler must document the reasons for the selection in the case record.
(7) Sometimes examination by more than one kind of specialist is required in order to fully address work-related injuries and any complications that may be associated with the injuries. If the CE has identified the need for examination by two kinds of specialists, for instance an orthopedist and a psychiatrist or clinical psychologist, the scheduler will arrange two separate examinations without asking either physician to coordinate the results.
On the other hand, a referral physician who needs to obtain information from another provider is authorized to make subsidiary referrals as necessary (for instance, a psychiatrist may refer a claimant to a clinical psychologist for testing). In this case, the referral physician should submit a summary report discussing any discrepancies among the physicians' viewpoints so that questions posed by OWCP are fully answered.
In extremely complex cases, a panel of physicians may be asked to examine the claimant and render a collective opinion. The services of such panels are most easily arranged through medical schools and hospitals, as these institutions employ specialists in many fields of medicine. Such referrals are rare.
c. Information Sent to Physician. The physician should be provided with the following:
(1) Description of the reason(s) for requesting the examination, including an indication of the conflict and a list of questions to be resolved, along with a blank Form OWCP-5 if appropriate.
(2) Statement of Accepted Facts (SOAF).
(3) Copy of the complete case file, either in paper or electronic form.
(4) Notice that he or she is the only individual authorized to perform the requested examination and provide the required report.
(5) Prompt payment billing information, including the code for referee medical examination or case review.
d. Information Sent to Claimant and Properly Authorized Designated Representative. Once the appointment has been scheduled, the claimant/representative should be notified. See Rosita Mahana, 50 ECAB 331 (1999) (ECAB held that by not notifying appellant and her attorney of the identity of the impartial medical specialist, OWCP deprived her of an opportunity to present any objections to the selection of Dr. Schwarz as the impartial medical specialist; and, accordingly, Dr. Schwarz was not properly selected as an impartial medical specialist and her report could not be used to resolve the conflict of medical opinion). The claimant and his or her duly appointed representative should be provided with the following information:
(1) Notice of the existence of a conflict in the medical evidence and the specific nature of the conflict. Notification should also be included that the examination is being arranged under the provisions of 5 U.S.C. 8123, which provides the claimant an opportunity to raise any objection to the selected physician prior to the examination.
(2) The name and address of the physician to whom he or she is being referred, as well as the date and time of the appointment.
(3) A warning that benefits may be suspended pursuant to 5 U.S.C. 8123(d) for failure to report for examination.
(4) Information on how to claim travel expenses.
e. The employee is not entitled to have anyone present at the examination unless OWCP decides that exceptional circumstances exist. For example, an interpreter may be allowed if a claimant is hearing-impaired. The law does not provide for participation by a physician of the claimant's choice in a referee examination (unlike second opinion examinations). 20 C.F.R. § 10.321(b).
f. A claimant who asks to participate in selecting the referee physician or who objects to the selected physician should be requested to provide his or her reason for doing so. The CE is responsible for evaluating the explanation offered. See Miguel A. Munitz, 54 ECAB 217, 221 (2002) (ECAB held that OWCP properly denied appellant's request to participate in the selection of the impartial medical specialist: "appellant's representative merely requested to participate in the selection of the referee examiner, in an 'attempt to assure that the claimant receives an impartial evaluation concerning this schedule award claim.' The Board finds that he did not provide a valid reason for participating in the selection and did not raise a specific objection to the selected physician."); Terrance R. Stath, 45 ECAB 412 (1994) (ECAB has recognized that under the OWCP's procedures, a claimant is entitled to participation in the selection of an impartial specialist; however, the claimant does not possess an unqualified right to participate. The claimant must provide a valid reason for request for participation at the time the conflict of medical opinion is found.).
(1) Examples of circumstances under which the claimant may participate in the selection include (but are not limited to):
(a) Documented bias by the selected physician;
(b) Documented unprofessional conduct by the selected physician;
(c) A female claimant who requests a female physician when a gynecological examination is required; or
(d) A claimant with a medically documented inability to travel to the arranged appointment when an appropriate specialist may be located closer. For instance, if the orthopedic specialist chosen through the Medical Management application in iFECS is three hours by automobile from the claimant's home, but an orthopedic specialist in the nearest large city is only one hour away by airplane, the latter physician may be chosen if the attending physician documents that the claimant can not travel for three hours by automobile.
(e) Simple preference for examination in a particular location will not be considered a valid reason. See S.W., Docket No. 09-1110 (issued February 19, 2010) (ECAB held that appellant did not present any evidence establishing that the impartial selection was improper: "Although appellant's attorney noted that the Office of the impartial medical examiner was approximately 281 miles from appellant's residence, the Office indicated that it would reimburse travel expenses, including the cost of an overnight stay, if necessary. A simple preference for examination in a particular location is not considered a valid reason for objecting to an impartial medical examiner.").
(2) If the reason is considered acceptable, the scheduler will prepare a list of three specialists available through the Medical Management application in iFECS, including a candidate from a minority group if indicated, and ask the claimant to choose one. This is the extent of the intervention allowed by the claimant in the process of selection or examination.
(3) If the reason offered is not considered valid, a formal denial on the claimant's request, including appeal rights, may be issued if requested.
g. Follow-up Action. Using the SOAF as the framework for his or her opinion, the referee physician should provide a report which contains a clinical history, results of the examination, results of any testing performed, and a reasoned opinion in response to the questions posed sufficient to resolve the conflict. A report should be expected within 30 days of the examination.
(1) If no medical report is received within 30 days from the date of appointment, the CE or medical scheduler should inquire as to the status with the referee physician's office. The CE or medical scheduler may also follow up soon after the date of the appointment to verify the claimant's attendance at the appointment. For a complete discussion describing the circumstances under which benefits may be suspended under 5 U.S.C. 8123(d) for failure to attend an appointment, see PM 2-0810-13 Suspension of Benefits.
(2) The CE must refrain from verbal contact to discuss any substantive issue in the case with a physician who has been engaged to provide a referee opinion. All such communication regarding these issues should be in writing.
If a referee medical report is obtained through such substantive telephone contact with the physician or submitted as a result of such contact, the referee report must be excluded. See PM 2-0810-12 for further details regarding exclusion of medical evidence.
The CE may only verify attendance at the appointment and inquire as to the status of the submission of the report, and should document that verification with a CA-110.
(3) Upon receipt of the report, the CE should review the specialist's report to ensure that it meets the requirements for a referee examination and that it addresses all issues posed.
(a) If someone other than the selected physician examined the claimant, the report cannot be used to resolve a conflict in medical opinion and cannot be afforded special weight. It should be annotated accordingly, and another referee examination must be arranged. Moreover, any indication of interference by the employing agency or claimant's representative will be considered sufficient to bias the report, which will then not be considered probative evidence.
(b) If clarification or additional information is necessary, the CE should write to the specialist to obtain it. Under no circumstances, however, should the CE telephone the specialist for elaboration of the report as information obtained in this manner cannot be considered probative medical evidence and bias may be inferred as a result, leading to exclusion of the report. See PM 2-0810-12 for further details regarding exclusion of medical evidence.
(c) Upon receipt of any clarifying information, the CE should again review the report to ensure that it is complete and pertinent to the questions asked. When the referee's report is considered adequate, the CE will take action without review by the DMA, except where a referee examination was arranged to resolve a schedule award issue. See PM 2-810-8.k. for further details regarding DMA review of referee reports relating to schedule award determinations.
Back to Chapter 3-0500 Table of Contents
5. Medical Management Application. The Medical Management application in iFECS, which replaced the Physician Directory System (PDS), allows users access to a database of Board-certified specialist physicians and is used to schedule referee examinations. On rare occasions, the Medical Management application will be used to locate qualified second opinion examiners if a second opinion examiner within the second opinion contract for the District Office cannot be utilized; the rotational requirement does not apply to second opinion examiners. The Medical Management application contains an automatic and strict rotational scheduling feature. This application provides for consistent rotation among physicians and records the information needed to document the selection of the physician.
a. In 2000, an updated version of the PDS stand-alone software was placed into the FECS system, replacing the previous PDS system. The directory of medical specialists contains physicians from the American Board of Medical Specialties (ABMS). The ABMS includes the medical Boards of the American Medical Association (AMA) that certify candidates in their respective fields of specialization.
The OWCP recognizes osteopathic doctors (D.O.) as physicians within the meaning of the Act. As such, the OWCP also accords special weight to their opinions as impartial referee physicians, provided they are Board-certified with the American Osteopathic Association (AOA).
b. Selection of a referee physician should be made only through the use of the Medical Management application (absent exceptional circumstances discussed below), and CEs may not dictate which physician will serve as a referee examiner.
However, where exceptional circumstances exist (such as when an esoteric specialty is required, or the Medical Management application does not contain any physicians of the required specialty within a 200-mile radius of the claimant's home zip code), scheduling outside of the Medical Management application may be appropriate. If this occurs, the scheduler should consult an appropriate directory of Board-certified medical specialists to obtain names of suitable physicians for referral. Documentation outlining the rationale for this decision must be placed in the case file, and the decision must be approved by a Supervisory Claims Examiner or higher level authority.
If an examination needs to be rescheduled with a prior referee examiner in accordance with a remand order or when a follow-up examination is necessary, scheduling outside of the strict rotational guidelines may also be necessary. In these more obvious instances, documentation must still be placed in the case file, but approval by a Supervisory Claims Examiner or higher level authority is not required.
c. When the medical scheduler inputs a claim number, the claimant's home zip code is automatically loaded. The medical scheduler then chooses the type of examination (generally referee) and the appropriate specialty. Information regarding the next physician on the roster, based on primary medical specialty and zip code, appears on the screen and remains on the screen only until the appointment is scheduled or until the physician is bypassed.
The entire roster of physicians is invisible to the medical scheduler, as he or she can only see and update appointment information pertaining to any particular physician while an attempt to schedule an examination with that physician is being made. See paragraph 6 of this chapter for a complete discussion on the reasons for bypassing a physician.
d. The universe of physicians included in the search and available for second opinion or referee scheduling is based on the primary specialty chosen and the claimant's home zip code.
e. Presentation of Physicians.
(1) The Medical Management application uses zip code clusters (the first three digits of the zip code) to select physicians for the initial rotation. For example, if the claimant's home zip code is 12345, the Medical Management application will select physicians of the appropriate specialty who have "123" as the first three digits in their zip codes.
(a) From the universe of physicians in this zip cluster, the Medical Management application separates them into essentially two groups – physicians who have previously had an appointment scheduled within the Medical Management application, and those who have not.
(b) The physicians who have not had a previous appointment scheduled in the Medical Management application are presented to the scheduler first. These physicians are presented in alphabetical order.
(c) If all of these physicians must be bypassed, then the Medical Management application presents the physicians who have had previous appointments scheduled. These physicians are presented in order such that the physician who had an appointment scheduled most recently will be at the bottom of the list based on the date that the last appointment was scheduled. The physician who had an appointment scheduled furthest in the past will be the first physician presented (after those who have never had a previous appointment scheduled).
Note that the order is based on the date on which the last appointment was scheduled (not the date of the actual appointment).
(2) If every physician in the initial zip cluster must be bypassed, the Medical Management application will then select physicians outside of the zip cluster that are within a 50-mile range of the claimant's home zip code. Physicians are presented in the same order as the initial zip cluster (first those who have never previously had an appointment scheduled within the Medical Management application, and then those that have had a previous appointment scheduled). See 5e(1) above.
If every physician in the 50-mile range outside of the zip cluster must be bypassed, the Medical Management application then extends to a 75-mile range, and continues to expand in 25-mile increments until the 200-mile range is reached.
(3) The Medical Management application sets 200 miles as the maximum limit for a zip code range.
(a) Once the 200-mile range (using the claimant's home zip code) has been exhausted, a "Zip Code Exhausted" report will be automatically generated for the file showing all of the physicians that have been bypassed during that search.
(b) If the scheduler reaches the 200-mile limit and still cannot locate an appropriate physician, the scheduler will then need to use an alternative method for scheduling the examination as outlined in 5b of this chapter. Alternatively, it may be appropriate to choose a different zip code, other than the claimant's home zip code, in order to continue the search. A different zip code may be used, for instance, if the claimant lives in a very remote area and will need to travel to a larger city in order to attend a scheduled examination. In this instance, the scheduler will enter the zip code of the city to which the claimant will be traveling.
(c) An alternative search with a different zip code should only be pursued if the 200-mile range (using the claimant's home zip code) has been exhausted. The reason for the alternative zip code search should be documented in the file.
(4) The Medical Management application calculates "distance" based upon the approximate number of miles between the claimant's home zip code and the physician's zip code. This "distance" is not a precise determination based upon a calculation from the claimant's specific address to the physician's specific address, since the capability to calculate that precise distance does not exist within iFECS.
Note that the "distance" need only be within the specified incremental range and does not affect the order in which the physicians are listed as described in 5e(1) above.
f. The medical scheduler will contact each physician presented by the Medical Management application to ascertain whether the necessary appointment can be scheduled in a timely manner.
g. If an appointment cannot be scheduled in a timely manner (or cannot be scheduled for some other reason such as a conflict, the physician is of the wrong specialty, etc.), the scheduler will update the application with an appropriate bypass code. Upon entering a bypass code, the Medical Management application will select the next physician in the rotation (as outlined in 5e above). See paragraph 6 of this chapter for more explicit information pertaining to the use of bypass codes.
h. If the physician agrees to schedule the appointment, the scheduler inputs the appointment date and time into the Medical Management application. The application saves the appointment information and prompts the scheduler to generate the ME023, Appointment Notification Report, for imaging into the case file.
i. The ME023, Appointment Notification Report, can only be generated through the Medical Management application and serves as documentary evidence that the appointment was scheduled through the use of the rotational system in the Medical Management application. The medical scheduler should image a copy of the ME023 report into the case file to substantiate that the rotational system was used to select the physician. In the event that the ME023 report is not imaged into the case file at the time the appointment was scheduled, and an issue is subsequently raised concerning the physician selection (such as in an appeal process), a copy of the original ME023 report may be reproduced at a later date.
Note, however, that the updated version of the ME023 report (described below) can only be generated for new appointments created on and after December 17, 2012. It cannot be accurately generated for appointments made prior to December 17, 2012, and the prior version of the ME023 report (without bypass information) can no longer be duplicated.
As of December 17, 2012, the ME023 report contains the following information:
(1) For the physician selected, the following information will be available on page 1 of the report: the claimant's name, case number, and home zip code; the name, address, phone number, and specialty of the physician selected for the appointment; the date, time, and type of appointment; and the user ID of the individual who generated the report.
If physicians were bypassed prior to the selection of this physician, the selected physician's information will also be listed at the end of the report in a section that denotes the physician that was selected for the appointment. The date on which the appointment was scheduled will also be listed here. (This is not the same as the date of the actual appointment.)
(2) For each physician bypassed, the report will show the following information on subsequent pages of the report:
(a) The name, specialty, state, and zip code based upon the information in the Medical Management application.
(b) A distance based on the approximate number of miles between the claimant's home zip code and that physician's zip code. See 5e(4) for more detail on the calculation of the distance.
(c) The date on which the last appointment was scheduled with that physician based upon the information in the Medical Management application. (This is not the same as the date of the actual appointment.) If there is no record of any previously scheduled appointment, the report will list "none."
(d) The date and time the physician was bypassed, along with the bypass code (and bypass note, if any). See paragraph 6 of this chapter for a more detailed discussion of bypass codes.
(3) Every page of the ME023 report (other than the first page) has a certification statement on the bottom verifying that the report is evidence that the appointment was scheduled using the Medical Management application in iFECS.
(4) The ME023 report is separated into sections based on the various search ranges (Initial Zip Cluster Match, 50-Mile Range Outside of Zip Cluster, 75-Mile Range Outside of Zip Cluster, etc.). If no physicians were found within a particular range, the report shows this result.
j. If a scheduled appointment has to be cancelled or rescheduled for any reason, the file should be appropriately and clearly documented.
Back to Chapter 3-0500 Table of Contents
6. Medical Management Codes. The Medical Management application has numerous codes to display the disposition of physicians and appointments.
If a physician cannot or will not schedule an examination, he or she must be bypassed in the Medical Management application so that the next physician in the rotation is available for scheduling. Various codes are used to document the reasons for not scheduling an examination with a physician in the rotation.
Most codes are stand-alone codes and do not require any rationale beyond their meaning as outlined in this chapter. However, three codes, code B (Busy), code L (Location), and code O (Other), do require a note explaining the reason for entry of the code. The note is entered directly into the Medical Management application, without any requirement that the imaged file be documented. Bypass notes entered must be sufficiently detailed to explain the reason the physician was bypassed (e.g. a note like "pass" is not sufficient), and the use of local abbreviations should be avoided. Finally, while notes are not mandatory for all codes, if the scheduler enters a note, it should be applicable and germane to the bypass code used.
Code A - Appointment Cancelled. This code is used when an appointment has been cancelled by either the physician or OWCP. This code is not a bypass code option but can be used in other portions of the Medical Management application.
Code B - Busy. This code is used when the physician cannot schedule an appointment in a reasonable amount of time (usually within 60 days) or is on extended leave or a leave of absence. A note is required to further explain usage of this code, e.g. "physician is on medical leave of absence - unknown return date." This code should NOT be used if the telephone line is busy or if the medical receptionist indicates the physician is too busy at the moment to take the call.
If a physician will be on a defined period for a leave of absence longer than 60 days, the user should annotate the physician's record in the Medical Management application in iFECS as appropriate. This will ensure that the physician does not appear in the rotation for the leave of absence period but will again appear in rotation once the leave of absence has ended.
Code C - Conflict. This code is used if the physician, or his/her associate, has a previous connection with the claim. This also includes physicians performing fitness for duty exams for the employing agency.
Code D - Physician does not accept DOL patients. This code is used if the physician will not accept any Department of Labor (DOL) cases, will not do IMEs, will not accept workers' compensation cases, or is not willing to perform examinations for OWCP.
If a physician will not accept DOL or OWCP cases for medical examinations, the physician's record in the Medical Management application in iFECS should be updated so that the physician no longer appears in the rotation.
Code E - Excluded/Lost license. This code is used if a physician is an excluded provider or has lost required licensing. This code is not a bypass code option but can be used in other portions of the Medical Management application.
Code L - Location is too far for claimant. This code is used when the physician's office is too far for the employee to travel, or the claimant may be medically unable to travel long distances to report for examination. A note is required to further explain usage of this code, since distance to travel is accounted for in the rotational presentation of physicians in the Medical Management application.
Code M - Physician moved out of zip code area. This code is used when the physician is no longer at the address shown in our database. The medical scheduler should attempt to obtain current contact information to update the physician address in the Medical Management application. If the physician is still within the same zip code as the address in the Medical Management application, the address can be updated and the appointment scheduled.
Code O - Other. This code is used when none of the other bypass reasons are applicable. This code is appropriate to use when no one answers the phone (e.g. "phone rings continuously with no answer") or the phone number has been disconnected (e.g. "phone disconnected/no other contact number noted"). A note is required to explain usage of this code, and code O should not be used if there is another appropriate code.
Code O is also appropriate if the medical scheduler must leave a message. If a message must be left, the medical scheduler should note the name of the person who was contacted or that a message was left on a voice mail. While waiting for a return call, the appointment with that particular physician should be put into a "pending" status. The scheduler should allow the physician's office a minimum of two business hours for a return call (as determined by usual physician business hours). If the physician's office does not call back within this period of time, the physician can be bypassed with the O code and another physician can be contacted. When the scheduler removes the "pending" status, the bypass note should be updated with an annotation that no call back was received. If a call back was received, and it was determined that the appointment could not be scheduled for some other reason (related to another bypass code), the record should be updated accordingly.
If a physician previously bypassed as non-responsive contacts the OWCP medical scheduler prior to the scheduler finalizing an appointment with another physician, continued efforts to arrange an examination with the second physician should cease and the appointment should be scheduled with the previously bypassed physician, as he or she was actually earlier in the rotation of physicians. If this occurs, the note should be updated accordingly when the appointment is scheduled.
Code S - Subspecialty. This code is used if the case requires a different subspecialty, or if the physician does not evaluate the specific body part or extremity. For instance, the physician will only perform exams for back conditions but the claimant has an upper extremity injury.
Code U - Physician in use by another user. This code is used when the physician is in use by another user. It is not available as a bypass option; rather, it is automatically updated by the Medical Management application when the next physician in the rotation is currently in use or in pending status (being contacted for an appointment) by another user.
Back to Chapter 3-0500 Table of Contents
|
Paragraph and Subject |
Date |
Trans. No. |
|---|---|---|
|
Table of Contents |
09/96 |
96-15 |
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
09/94 |
94-42 |
|
|
09/95 |
95-39 |
|
|
12/91 |
92-07 |
|
|
10/90 |
95-04 |
|
Exhibits |
|
|
|---|---|---|
|
1. Attending Physician's Report, Form CA-20 |
12/94 |
95-04 |
|
2. Attending Physician's Supplemental Report, Form CA-20a |
12/94 |
95-04 |
|
|
|
|
|
3. Duty Status Report, Form CA-17 |
12/94 |
95-04 |
|
|
|
|
|
09/96 |
96-15 |
|
|
5. Outline for Otologic Evaluation, Form CA-1332 |
09/94 |
94-42 |
|
09/94 |
94-4 |
|
|
7. OWCP Medical Examination Requirements in Asbestos Disease Cases |
12/94 |
95-04 |
|
8. Roentgenographic Interpretation, Form CM-933 |
12/94 |
95-04 |
|
|
|
|
|
|
|
|
|
12/94 |
95-04 |
1. Purpose. The Office relies on written medical reports to justify awards for compensation, support payment of medical expenses, and monitor the quality of care being provided. This chapter will detail the type of information needed to render proper determinations for the medical issues in each case.
Back to Chapter 3-0600 Table of Contents
2. Reports of Disability and Impairment. Reports are submitted by attending physicians, consultant (second opinion) specialists, and referee physicians. Each report may address one or more topics pertaining to the claimant's medical status. Whatever the format or source of a report, the information provided in it must be sufficiently clear and detailed so that claims and medical reviewers are certain of the physician's findings, conclusions, and opinions.
Under the FECA, impairment is defined as the anatomical or functional loss or reduction of a function of an organ of the body in reference to the activities of normal life; it pertains solely to the claimant's medical condition. Disability is defined, on the other hand, in terms of the claimant's ability to perform the duties of his or her job.
Back to Chapter 3-0600 Table of Contents
3. Statement of Accepted Facts (SOAF). Where a medical opinion is needed to resolve an issue in a case, the file is referred to the Medical Unit with a list of questions (see paragraph 4 below). An SOAF usually accompanies the case and provides the factual background for the physician's opinion. Only where the Claims Examiner (CE) needs general information, for instance about the course of a disease, will an SOAF not be included.
a. Contents. All SOAFs should include the information listed in items (1) through (6); depending on the issue to be resolved, the information shown in items (7) though (10) will be included as well:
(1) The claimant's name and age;
(2) The employer and the job held at the time of injury;
(3) Mechanism of injury;
(4) Conditions claimed or accepted;
(5) Work history since the injury, including the date the claimant stopped work and returned to either light or regular duty;
(6) A description of medical treatment since the injury, including dates of treatment and names of physicians, and if relevant what diagnostic tests were conducted (physicians' findings and conclusions should not, however, be discussed in the SOAF);
(7) Relevant medical history;
(8) Specific description of injury or exposure factors, particularly in cases involving occupational disease;
(9) The claimant's hobbies or activities outside of work;
(10) Physical or mental demands of claimant's regular or light duty job, or of light duty job offered.
Detailed instructions for CEs concerning the preparation of SOAFs are contained in PM Chapter 2-809.
The CE is responsible for ensuring that the SOAF is correct, complete, unequivocal, and specific. When the DMA, second opinion specialist or referee physician renders a medical opinion based on an SOAF which is incomplete or inaccurate or does not use the SOAF as the framework in forming his or her opinion, the probative value of the opinion is seriously diminished or negated altogether.
Back to Chapter 3-0600 Table of Contents
4. Questions for Response. Files referred to the Medical Unit will contain a list of question composed by the CE for response by the physician (DMA, second opinion or referee) to answer. In reviewing case files, the DMA should ensure that he or she addresses each of the questions posed, preferably in the order given, and that the response is:
a. Complete and accurate in addressing all of the questions posed and in addressing them thoroughly. In some instances the DMA may identify medical issues which the CE has not addressed. It is perfectly appropriate to discuss such issues and provide information in addition to what the CE has requested as long as medical rather than adjudicatory questions are the subject of the discussion.
b. Responsive to the material provided in the SOAF. If the physician whose reports are under review has based his or her opinion on other factual material, the DMA should take account of this in reaching an opinion.
c. Well rationalized in discussing the opinion reached. Because the quality of the Office's adjudicatory functions depends heavily on well reasoned medical evidence, it is very important to provide clear rationale for the opinion given.
d. Neutral with respect to adjudicatory issues. It is not appropriate for the DMA to offer opinions as to whether a case or medical condition should be accepted. Doing so may adversely affect the outcome of the case since it may suggest bias to a later reviewer.
Back to Chapter 3-0600 Table of Contents
5. Form of Medical Reports. The DMA will be expected to review, interpret, or evaluate a variety of medical reports ranging from simple form reports to detailed narrative reports (it should be noted that the use of an OWCP form is never required in making reports). Descriptions of OWCP forms are as follows:
a. Form CA-16, Form CA-20, and Form CA-20a, Attending Physician's Report. An initial or preliminary report may be submitted on either Form CA-16 (Exhibit 1, Chapter 3-300 (Link to Image)) or Form CA-20 (Exhibit 1 Pages 1-2( Link to Image); Page 3 (Link to Image)), while a supplementary report may be submitted on Form CA-20a (Exhibit 2 (Link to Image)). A completed Form CA-16 or CA-20 represents sufficient medical evidence for adjudication of most traumatic injury claims, although additional evidence in narrative form may be required to justify payment of continuing benefits.
b. Form CA-17, Duty Status Report. The CA-17 (Exhibit 3 (Link to Image)) is used by the employing agency to obtain information from the attending physician about the claimant's work restrictions. A copy of the form may be sent to OWCP to aid in evaluating the extent of disability remaining. Reports submitted by the employing agency generally do not address all pertinent issues such as the causal relationship between current disability and factors of Federal employment. Therefore, these reports are usually considered as supplemental information although some narrative fitness-for-duty reports may be sufficiently probative in and of themselves.
c. Narrative Report. A narrative medical report may be required if disability continues or complex issues such as a pre-existing medical condition are present. In addition, narrative reports are necessary in almost all occupational disease cases. In any case where the injury causes disability for work for an extended period or requires lengthy treatment, reports describing the clinical course, prognosis, and recommendations for further medical care must be furnished as needed.
Back to Chapter 3-0600 Table of Contents
6. Content of Medical Report. Regardless of the form a medical report takes, the following information will usually be required:
a. Dates of examination or treatment;
b. Clinical history given to the physician;
c. Detailed description of physical findings;
d. Results of any x-ray or laboratory tests;
e. Diagnosis;
f. Prognosis;
g. Description of impairment, if any;
h. Specific limitations for work;
i. Clinical course of treatment followed;
j. The physician's reasoned opinion as to the relationship between the condition found and factors of Federal employment. (Causal relationship is discussed in PM Chapter 2-805.)
In addition, a detailed description of the employee's work tolerance limitations is required in any case where the issue is the claimant's ability to return to duty, and a detailed description of anatomical impairment in accordance with the AMA Guides is required in any claim for schedule award.
Back to Chapter 3-0600 Table of Contents
7. Criteria. Guidelines for weighing the value of medical reports are provided in PM Chapter 2-810. The Office uses the following criteria in evaluating medical opinions:
(1) Physician's Qualifications. The opinion of a specialist in the appropriate field of medicine often carries greater weight than the opinion of a non-specialist or a specialist in an unrelated field. The opinion of a Board-certified specialist or a specialist of professorial rank will carry added weight.
(2) Medical Rationale. Opinion supported by a medical explanation is required in most cases.
(3) Accuracy and Completeness. The factual and medical background reflected in the report must be correct and complete in accordance with the facts of the case and the medical information reflected in other reports in file.
(4) Comprehensiveness. A comprehensive report is one which reflects that all testing and analysis necessary to support the physician's conclusions have been performed.
(5) Consistency. The physical findings must substantiate the medical opinion.
(6) Decisiveness. Opinions containing unclear or vague language can be characterized as equivocal, speculative or conjectural. Terms such as "could", "may", or "might be" indicate speculation and/or equivocation and are assigned less probative value than positively expressed medical opinions. The term "probably" is considered less speculative than the above terms and therefore has greater probative value.
The DMA should render his or her opinion using the Statement of Accepted Facts (SOAF), which the CE prepares (see Chapter 3-500 for a discussion of the SOAF). The opinion should be based on the medical evidence of record (except for any reports annotated with the word "excluded" because the evidence which they contain was improperly obtained.) The DMA should avoid commenting on legal issues when rendering a medical opinion. If the DMA disagrees with the opinion of the treating physician, a clear and thorough medical explanation must be included.
Back to Chapter 3-0600 Table of Contents
8. Specific Conditions. OWCP has developed checklists for use by claimants and their official superiors in order to better identify and gather the information required to support a claim for occupational disease. These checklists address the following conditions: hearing loss, asbestos, coronary/vascular conditions, skin diseases, pulmonary disease other than asbestos, psychiatric illness, and carpal tunnel syndrome. A general checklist is also available for use in claims for occupational diseases not enumerated above.
Occupational disease claims in general are discussed in PM Chapter 2-806. The following guidance is provided with respect to specific medical conditions encountered in OWCP claims:
a. Hearing Loss. Refer to "Medical Management of Claims under the FECA" for a discussion of development of such cases. It is generally accepted that hearing loss may result from prolonged exposure to noise levels above 85 decibels. Acoustic trauma may, however, result from decibel levels below 85 decibels if exposure is sufficiently prolonged. OWCP therefore does not require that the claimant show exposure to injurious noise in excess of 85 decibels as a condition to approval of the claim.
(1) After obtaining all pertinent factual evidence, the CE will prepare a Statement of Accepted Facts. Unless the case file already contains a reliable medical report which fully meets OWCP requirements, the CE should refer the claimant for audiological evaluation and otological examination which addresses the relationship of any hearing loss to the employment and the degree of any permanent impairment.
The audiological evaluation and the otological examination are to be performed by different individuals as a method of evaluating the reliability of the findings through independent observations. If possible, the two consultations should occur on the same day. The usual information sent to consultants, as outlined in PM 3-500.3c, should be forwarded to both the audiologist and otolaryngologist.
(2) The audiological testing is to be performed by persons possessing certification in audiology from the American Speech-Language-Hearing Association (ASHA), or State licensure as an audiologist. The audiological testing should precede the visit to the otolaryngologist since the latter should have the audiological findings at the time of the examination. The audiological examination should be conducted in accordance with OWCP requirements, which are described in Form CA-1087 (Exhibit 4).
(3) The medical examination should be performed by an otolaryngologist certified (or eligible for certification) by the American Board of Otolaryngology. The physician should be instructed to conduct additional tests or retests in those cases where the initial tests were inadequate or there is reason to believe the claimant is malingering. Form CA-1331 and Form CA-1332 can be used to obtain the required report.(Exhibit 5) Pages 1-2 (Link to Image); Pages 3-4 (Link to Image))
(4) Audiological equipment used for testing must meet the calibration protocol embodied in the Professional Services Board Manual of the ASHA (see Exhibit 6). Each audiologist or physician who conducts hearing tests must certify that at the time of examination the equipment used for testing met the standards for accreditation of an audiological facility by ASHA (ANSI S 3.6 (1969) and 3.1 (1977), respectively).
(5) Where the employee is deceased, the following procedures are to be followed according to the stage of development of the medical evidence:
(a) Where an audiogram meeting the requirements set forth in Form CA-1087, either alone or in conjunction with audiograms that do not meet OWCP requirements, appears in the file, the audiogram may be used as the basis of an award if it is medically determined to be internally consistent (the various measurements of the components of hearing are in substantial agreement) and the evidence shows a causal relationship between the hearing loss and employment.
(b) Where no audiogram meets the requirements of Form CA-1087, an audiologist should review all audiograms in the case to ascertain whether they are internally consistent with each other and whether the hearing loss was causally related to employment. If so, an appropriate audiogram should be selected as the basis for an award. If not, every effort should be made to determine an equitable award. Where an award is made based on evidence which does not fully meet the OWCP's requirements, the CE should prepare a detailed memorandum to the file which explains how the award was determined. Such decisions should be signed at the level of the Senior CE or above.
(6) The DMA calculates the percentage of hearing loss using Form CA-51 (see Exhibit 3 of PM 3-700 (Link to Image,)) if a schedule award is at issue. The DMA provides opinion regarding the causal relationship between any hearing loss and the employment and verifies the calculations of the audiologist.
b. Asbestos-Related Diseases. Refer to "Medical Management of Claims under the FECA" for a discussion of development of such cases. It is accepted that asbestos-related disease may result from occupational exposure in excess of two fibers/cc (moderate or heavy) during the course of Federal employment, or the presence of asbestos dust on work surfaces, even if invisible.
(1) After obtaining all pertinent factual evidence, the CE should consider referral to a pulmonary specialist.
(a) If the level of exposure indicated above has been met and a medical report indicates the possible existence of an asbestos-related abnormality, such as X-ray report of pleural or parenchymal abnormality or report of pulmonary fibrosis, the CE should prepare a Statement of Accepted Facts and arrange for referral of the claimant to a pulmonary specialist for complete evaluation in accordance with the requirements shown in Exhibit 7, OWCP Medical Examination Requirements in Asbestos Disease Cases.
(b) If the level of exposure indicated above has been met but no medical report indicates the possible existence of an asbestos-related abnormality, the claimant shall be instructed to arrange for submission of a current medical report from his or her treating physician which meets all of the requirements shown in Exhibit 7, OWCP Medical Examination Requirements for Asbestos Disease Cases. If the submitted report satisfies OWCP requirements and the case is accepted, the cost of the examination is reimbursable.
In addition to the usual materials sent to consultants (see PM 3-500.3), the physician selected should be sent copies of Form CM-933 (Exhibit 8, Page 1 (Link to Image), Page 2 (Link to Image)) and the job description.
(2) Where the employee is deceased, the CE should evaluate the available medical evidence for completeness and refer the file for medical evaluation (with Statement of Accepted Facts) to a pulmonary specialist.
(3) The DMA or consultant acting in that capacity, preferably a Board-certified pulmonary specialist, should review the report once the CE determines that it is complete. The medical specialist should be asked to consider the following issues:
(a) Diagnosis. Are the laboratory and physical findings adequately supportive?
(b) Work-Relatedness. Has Federal occupational exposure contributed to development of diagnosed conditions by direct cause, aggravation, acceleration or precipitation?
(c) Impairment. With reference to the AMA Guides, what percent of pulmonary impairment is indicated?
(d) Disability. Is the evidence sufficient to allow a determination of the extent and degree of disability for normal work (current or last) as a result of the diagnosed condition? Is the disability partial or total, temporary or permanent?
(e) Treatment. Is the recommended treatment appropriate?
(f) Follow-up. When should the next pulmonary evaluation be performed?
(g) Employment. If the claimant is still employed and exposed to asbestos, should employment continue based on current medical findings, medical knowledge, and documented working conditions?
c. Carpal Tunnel Syndrome. This condition involves the compression of the medial nerve between the longitudinal tendons of the wrist musculature and the transverse superficial carpal ligament along the palmer aspect of the wrist (see Exhibit 9 (Link to Image)). Symptoms resulting from this compression include pain, numbness, tingling, and weakness of the affected hand (usually the dominant one, though bilateral involvement does occur). Causes which may be work-related include constant exertion and/or repetitive motion with the wrist flexed or extended against resistance, and acute trauma. The medical report should contain clear evidence that the disease is present. Among the clinical findings are:
(1) Phalen's Sign. This test is positive if maintenance of forced hyperflexion for one minute precipitates pain and paresthesia.
(2) Tinel's Sign. This test is positive if tapping over the medial nerve at the wrist produces pain.
(3) Neurological Abnormalitiesm. These include decreased sensation over the palmar aspect of the end joints of the same three and one half digits and atrophy of the thenar eminence in severe cases.
(4) Decreased nerve conduction velocity (NCV) as measured during nerve conduction test. The test results should include an evaluation as to whether the velocities obtained are normal or not.
(5) Decreased muscle motor activity as measured by electromyography (EMG). The test results should clearly indicate whether the results are within normal limits or are abnormal. An opinion as to the cause of the abnormality may also be present.
Back to Chapter 3-0600 Table of Contents
9. Partial Disability. When employment-related injury or disease permanently prevents a return to regular duties, the Office and the employing agency work together to reemploy the claimant within his or her work restrictions if possible. If not, OWCP will offer rehabilitation services to the employee with the goal of reemployment in the general work force.
a. Loss of Wage-Earning Capacity (LWEC). The CE monitors medical reports to determine the extent of disability resulting from an employment-related injury or disease. When an attending physician's report indicates the claimant is no longer totally disabled for all work, the physician is sent Form CA-1302, Request for Medical Progress Report (or narrative equivalent) and/or Form OWCP-5, Work Tolerance limitations. When this information is received, the DMA will review it in conjunction with the description of the position under consideration in order to determine the claimant's ability to perform the duties involved, if that position has been identified by using the Dictionary of Occupational Titles (that is, the position is not one which has actually been offered to the claimant).
Occasionally the DMA will be asked to complete the Form OWCP-5 based on the examining physician's findings. In doing so, the DMA should consider any disability which existed prior to the injury as well as any disability resulting from the employment injury. Subsequently acquired conditions unrelated to the injury are excluded from consideration in determining the claimant's LWEC but are included when considering suitability of an offered position.
b. End of Schedule Awards. As with disability, permanent impairment does not always result in a loss of wage-earning capacity. In some cases, however, the claimant cannot return to the kind of work performed at the time of injury, and when this happens, compensation may be awarded based on the claimant's LWEC. Prior to the expiration of the schedule award, the CE may request a current medical report to determine whether a claimant has any LWEC due to the employment injury. To make a proper determination, the DMA must review the claimant's job description, including its physical requirements, and compare the claimant's current work tolerance limitations with the position description.
Back to Chapter 3-0600 Table of Contents
Exhibit 1: Attending Physician's Report, Form CA-20
Page 1-2 (Link to Image)
Page 3 (Link to Image)
Back to Chapter 3-0600 Table of Contents
Exhibit 2: Attending Physician's Supplemental Report, Form CA-20a
Back to Chapter 3-0600 Table of Contents
Exhibit 3: Duty Status Report, Form CA-17 (Link to Image)
Back to Chapter 3-0600 Table of Contents
Exhibit 4: OWCP Hearing Loss Medical Requirements
OWCP HEARING LOSS MEDICAL REQUIREMENTS
Each employee should be seen for audiological and otological examination. The audiological testing should precede the visit to the otologist; the otologist should have the audiological findings at the time of the examination; and, to the extent possible, these two consultations should occur on the same day. It is also required that the audiological and otological examinations be performed by different individuals.
Any tests administered as part of an audiological battery must be conducted by a person possessing certification in audiology from the American Speech-Language-Hearing Association (ASHA) or State licensure as an audiologist. The medical examination must be performed by an otolaryngologist certified (or eligible for certification) by the American Academy of Otolaryngology. All tests comprising the battery administered in the audiological evaluation must be performed in an environment meeting the specifications of ANSI S3.1 (1977). Facilities which are accredited by the Professional Service Board of the ASHA meet this requirement. Testing equipment must be calibrated in accordance with the protocol contained in the accreditation manual of ASHA's Professional Service Board (ANSI S3.6-1969).
Audiometric tests must include the following:
1. Pure-tone air conduction thresholds should be obtained for each ear at 500, 1000, 2000, 3000, 4000, 6000 and 8000 Hz. Bone conduction thresholds should be obtained for the specified frequencies from 500 to 4000 Hz, inclusive. Appropriate masking should be employed as necessary and the use of masking should be denoted on the audiogram. The symbols used in recording thresholds should be in accordance with the most recent ASHA recommendations.
2. Impedence audiometry should be done on both ears as a means of determining the reliability of air-bone conduction threshold relationships and for any contribution it might otherwise make to differential diagnosis by the physician.
3. Speech reception thresholds for each ear should be established, using test procedures and spondaic words which conform to guidelines (ASHA Committee on Audiometric Evaluation, 1979). Standardized recorded materials should be used rather than live voices.
4. Monaural discrimination scores should be obtained; masking should be used when necessary. Standardized recorded word lists should serve as the stimuli and the discrimination scores for the full list should be reported for each ear.
Reports must include, as appropriate:
1. Date and hour of examination.
2. Date and hour of employee's last exposure to loud noise. (If the employee was exposed to noise within the last 16 hours, do not proceed with testing.)
3. History of injury.
4. The physician's rationalized medical opinion regarding the relation of the hearing loss to employment-related noise exposure.
5. The physician's recommendation for treatment.
6. A certification must accompany each audiological battery indicating that instrument calibration and the environment in which the tests were conducted met the accreditation standards of the Professional Services Board of ASHA (ANSI S3.6 (1969) and S3.1 (1977), respectively). A copy of the calibration standards are attached for your convenience.
7. A statement commenting on the reliability of the tests.
Back to Chapter 3-0600 Table of Contents
Exhibit 5: Outline for Otologic Evaluation, Form CA-1332
Pages 1-2 (Link to Image)
Pages 3-4 (Link to Image)
Back to Chapter 3-0600 Table of Contents
Exhibit 6: Calibration Requirements for Accreditation of an Audiological Facility by the Professional Services Board
CALIBRATION REQUIREMENTS FOR ACCREDITATION OF AN
AUDIOLOGICAL FACILITY BY THE PROFESSIONAL SERVICES BOARD
|
7.3.4. Calibration: The program shall establish and follow |
|
|
7.3.4.1. |
The program shall keep an accurate record of all audiometric calibrations performed. The record shall include at least: |
|
7.3.4.2. |
Diagnostic audiometers and/or audiometers used in fixed locations shall meet ANSI S3.6-1969 specifications for wide-range audiometers and shall be calibrated according to the following schedule: (1) A detailed biological check of the audiometer which includes a careful listening test of earphones and bone vibrator shall be performed to ensure that the audiometer displays no evidence of: (i) Cross talk. (2) An electroacoustic calibration check of non-solid-state audiometers shall be made once a month which includes at least the following measurements: (i) The accuracy of the sound presure levels for all pure tones in both earphones. c. Quarterly: An electroacoustic calibration check of solid-state audiometers shall be made once every three months which includes at least the measurements specified in section 7.3.4.2.(2)(i)through (iv). d. Annually: An electroacoustic calibration check of all audiometer shall be made every 12 months which includes at least the following measurements: (1) The accuracy of output levels for all pure tones in bone vibrator(s). |
Back to Chapter 3-0600 Table of Contents
Exhibit 7: OWCP Medical Examination Requirements in Asbestos Disease Cases
OWCP MEDICAL EXAMINATION REQUIREMENTS IN ASBESTOS DISEASE CASES
1. Occupational History. Chronological summary of the individual's job history which includes a description of the frequency, degree, and duration of occupational exposures to asbestos with emphasis on exposure in Federal civilian employment, but which includes exposure in non-Federal employment. Include other dusts or toxins and any non-occupational exposure.
2. Medical History. Chronological summary which includes references to any previous injuries or illnesses, pulmonary problems and the development of pulmonary symptoms. Summary of pulmonary symptoms. Complete smoking history. Family medical history.
3. Physical Examination. To include description of all the following:
a. General appearance and performance.
b. Sex, age, height and weight.
c. General examination denoting the presence or absence of cyanosis, clubbing, nicotine stains, edema, hepatomegaly, ascites and other signs ascribable to the pulmonary and cardiovascular systems.
d. The pattern and rate of claimant's breathing (presence and degree of dyspnea, etc.); the presence of any exertional changes.
e. Results of cardiac examination.
f. The results of chest examination, including configuration, findings on percussion and ausculation (i.e., the presence or absence of rales and/or other abnormal sounds).
4. Chest X-rays and CAT Scans. Minimum of AP, lateral and R and L oblique views. A full size x-ray shall be taken under the supervision of a Board-certified radiologist and read by either a Board-certified radiologist or pulmonary specialist. This reading must include a description of the quality of the film and all radiographic findings. The examining physician will also review the film for these same purposes.
The x-ray interpretation must include a description of any abnormality or pathology present with special attention given to evidence of pulmonary hypertension, fibrosis, carcinoma, or mesothelioma. If any abnormality or pathology is present, the description must include the following information:
a. Presence or absence of opacities described by type, size, shape, distribution and profusion.
b. Presence or absence of plural thickening, plaques or calcification, with description of site and extent.
c. Presence or absence of ill-defined diaphragmatic or cardiac outlines with description of extent.
d. Any other pertinent findings of a chronic or acute nature.
X-rays should be kept available for review but should not be sent to this Office unless requested. Additional views may be obtained at the discretion of the physician.
In lieu of x-rays, the physician may elect to perform computerized axial tomography (CAT scan) of the thorax, which can provide a more definitive view of the lungs and the presence or absence of asbestosis.
5. Pulmonary Function Studies. To include measurement of the following functions (the report of the results of the FVC, FEV(1), and diffusing capacity must include actual recorded values, the percent of predicted normal, and identification of the normal standard applied for tests conducted before and/or after the use of bronchodilators). These studies should be performed under the supervision or direction of a Board-certified pulmonary specialist.
a. Forced Vital Capacity (FVC) and Forced Expiratory Volume in One Second (FEV(1)) measured in liters and representing the best of three efforts and the FEV(1)/FVC Ratio (FEV(1)%) computed from these results. Also include total lung capacity (TLC). Report of the results of these tests must include:
(1) Date and time of the test.
(2) Name, file number, sex, age, weight, and height of the patient.
(3) The names of the technician performing and the physician supervising the test, if different from the referring physician.
(4) A description of the patient's ability to understand and follow instructions and the degree of cooperation in performing the test.
(5) The paper speed (if applicable) and the name of the instrument used.
(6) The date of last calibration of the instrument.
(7) Whether and why a bronchodilator was used and its impact on test results.
The report must be accompanied by appropriately labeled spirometric tracings (for all tests) showing distance per second on the abscissa and distance per liter on the ordinate.
b. Carbon Monoxide Diffusing Capacity (Single Breath Method). The results must be reported in ml/mm/mmHg. The report of the test must include estimated alveolar volume (based on measured FRC), the barometric pressure at the time of the test, the name of the technician performing the test and the instrument used, and the date of last calibration.
c. Arterial Blood Gas Study, administered at rest. A blood gas study may be done during exercise only if not medically contraindicated and if, in the opinion of the examining physician, it is necessary for diagnostic purposes. Report of the ABG study must include recorded values for pCO(2), pO(2), and pH collected simultaneously; the date and time of the test; the altitude and barometric pressure at which the test was conducted; the name of the technician and supervising physician; the pulse rate at the time the blood sample was drawn; the time elapsed between drawing and analysis of the sample and whether the specimen was iced; the duration and time of exercise (if appropriate); and a statement indicating that the equipment was calibrated before and after each test.
6. Electrocardiogram results submitted with tracings.
7. Complete Blood Count.
8. Medical Impression and Opinion which includes:
a. Diagnosis of all pulmonary conditions present.
b. Diagnosis of any other relevant disease condition present.
c. Recommendations regarding indicated course of treatment to improve the level of pulmonary function.
d. A discussion of the findings regarding the indicated degree of pulmonary impairment and exertional limitations (with reference to the enclosed job description).
e. Discussion of work-relatedness, including a detailed discussion of other possible etiological factors for each of the diagnosed conditions.
Back to Chapter 3-0600 Table of Contents
Exhibit 8: Roentgenographic Interpretation
Page 1 (Link to Image)
Page 2 (Link to Image)
Back to Chapter 3-0600 Table of Contents
Exhibit 9: Carpal Tunnel Cross-Sectional View (Link to Image)
Back to Chapter 3-0600 Table of Contents
|
Paragraph and Subject |
Date |
Trans. No. |
|---|---|---|
|
Table of Contents |
01/10 |
10-04 |
|
01/10 |
10-04 |
|
|
01/10 |
10-04 |
|
|
01/10 |
10-04 |
|
|
01/10 |
10-04 |
|
|
01/10 |
10-04 |
* (ENTIRE CHAPTER REISSUED 01/10, TRANSMITTAL NO. 10-04)
|
Exhibits |
Date |
Trans. No. |
|---|---|---|
|
1. Use of the Sixth Edition of AMA Guides to The Evaluation of Permanent Impairment |
01/10 |
10-04 |
|
01/10 |
10-04 |
|
|
01/10 |
10-04 |
|
|
01/10 |
10-04 |
1. Purpose. The FECA provides that compensation may be paid for total or partial loss, or loss of use of, certain parts of the body which are specified in the FECA itself and in the regulations. The purpose of this chapter is to describe the procedures involved in medical evaluation of claims for such awards.
Back to Chapter 3-0700 Table of Contents
2. Definition and Standards for Evaluation. The phrase "permanent disability" in 5 U.S.C. 8107(a) is interpreted to mean "permanent physical impairment." The same standards for evaluating such impairment are applied in all cases. The AMA Guides to the Evaluation of Permanent Impairment is used in order to provide a consistent method of calculating impairment. Exhibit 1 addresses calculations according to the Sixth Edition of the Guides.
Since the Sixth Edition of the Guides is diagnosis based, the main factor in determining impairment is the diagnosis itself. Each diagnosis grid is divided into five classes of impairment severity, ranked from '0' (no impairment) to '4' (very severe). Raters distinguish the level of severity using criteria separated into key factors and non-key factors. These criteria consist of: (1) history of clinical presentation; (2) physical findings; (3) clinical studies or objective test results; and (4) functional history. All of these various factors affect the total amount of impairment awarded to an individual.
Back to Chapter 3-0700 Table of Contents
3. Determining Schedule Awards. Development of cases for schedule awards is discussed in PM Chapter 2-808. The Claims Examiner (CE) will ask the District Medical Advisor (DMA) to evaluate a case when it appears to be in posture for schedule award determination. The DMA is responsible for reviewing the file, particularly the medical report on which the award is to be based, and then calculating the award. A table showing the number of weeks of compensation payable for various percentages of loss is shown as Exhibit 2.
a. Evaluating the Medical Report. The DMA should review the report of the physician estimating impairment with respect to the following factors:
(1) Maximum Medical Improvement. Before an award may be made, it must be medically determined that no further improvement can be anticipated and the impairment must reach a fixed and permanent state, which is known as Maximum Medical Improvement (MMI).
(a) While additional medical treatment (such as surgery) may be recommended in order to improve the claimant's condition, the claimant is not required to undergo such treatment. See Santo Panzica, 13 ECAB 458 (1964). The Office must calculate the percentage of the award as if no further improvement were possible if the claimant declines such intervention.
(b) It is well settled that maximum medical improvement arises at the point at which an injury has stabilized and will not improve further. This determination is factual in nature and depends primarily on the medical evidence. See Peter C. Belkind, 56 ECAB 580 (2005). Neither temporary nor future impairment may be rated. Impairment should not be rated permanent until sufficient time has passed for healing and recovery, which may vary substantially depending on the condition and the claimant. Clinical findings must indicate the medical condition has stabilized. See Franklin Armfield, 28 ECAB 445 (1977). A schedule award may be payable based on contemporaneous medical evidence of record showing a peak or plateau in the claimant's recovery status, even if the claimant's condition is likely to deteriorate. Payment of an increased award based on additional impairment may be considered at a later date.
(c) In the absence of evidence to the contrary or a conflict in the medical evidence requiring resolution under 5 U.S.C. 8123, the date of MMI is usually considered to be the date of the attending physician's evaluation that is accepted as definitive by the Office.
(2) Description of Impairment. The attending physician should describe the impairment in sufficient detail to permit clear visualization of the impairment and the restrictions and limitations which have resulted. The description should include the loss in degrees of active and passive motion of the affected member or function, the amount of any atrophy or deformity, disturbance of sensation, or other pertinent description of the impairment. Under the Sixth Edition of the AMA Guides, clinical history is also important in the diagnosis-based grid that ranks impairment within classes of severity.
(3) Percentage of Impairment. Impairment evaluation results are provided in terms of percentage of loss of use to the affected member or function of the body (not the body as a whole, except where impairment to the lungs and other bodily organs is at issue; see paragraph 4 below). The percentage should include those conditions accepted by OWCP as job-related and any pre-existing permanent impairment of the same member or function. If the work-related injury has affected any residual usefulness in whole or in part, a schedule award may be appropriate. There are no provisions for apportionment under the Act. Rated impairment should reflect the total loss as evaluated for the schedule member at the time of the rating exam. See Raymond E. Gwynn, 35 ECAB 247, 253 (1983) [In determining the amount of a schedule award for a member of the body, pre-existing impairments are to be included, citing Larson for the proposition that "the employer takes the employee as he finds him."]
b. Calculation. The DMA should use the method of calculation set forth in the AMA Guides. If it is necessary to deviate from the AMA Guides in calculating an award, the record should reflect the basis for the deviation, particularly when the use of a different table or evaluation materially affects the percentage of the award. The policy of the Office is to round the calculated percentage of impairment to the nearest whole point. Results should be rounded down for figures less than .5 and up for .5 and over.
Back to Chapter 3-0700 Table of Contents
4. Special Determinations. Following are guidelines under §8107 of the Act for calculating schedule awards for specific conditions:
a. Loss of Digits. While the percentage of impairment to the fingers is generally computed in accordance with the AMA Guides, special computations may be required. In general, loss of more than one digit should be computed in terms of impairment to the whole hand or foot. The impairment computed for loss of two or more digits occasionally exceeds the percentage for the hand or foot, however, and in such instances the award should reflect the computation most favorable to the claimant.
(1) Loss of Less Than One Phalanx. If less than one-half of a phalanx has been amputated but some loss of bone or bony tuft has occurred, the award shall be one-half of the amount payable for the loss of the first phalanx or for 25 percent of the digit. If more than half of a phalanx is lost, the award shall be for the entire loss of the first phalanx, or for 50 percent of the digit.
Where significant amputation of the soft tissue of the tip of the first phalanx has occurred with no loss of bone or bony tuft, the award shall be one-fourth the amount payable for the loss of the first phalanx or 13 percent of the digit.
If the injury has caused impairment such as loss of flexion or extension, swelling, gross deformity and/or changes in sensation in addition to the amputation, the additional impairment must be considered in the overall determination.
(2) Loss of Two or More Digits of a Hand or Foot. When there is a loss of two or more digits, or one or more phalanges of each of two or more digits, the award is proportional to the loss of use of the hand or foot.
By statute, the loss of one phalanx will be considered equal to 50 percent of the digit and loss of more than one phalanx will be considered equal to 100 percent of the digit. See 5 U.S.C. 8107 (15). The value of each digit lost will then be applied to the hand or foot in accordance with the AMA Guides. If the injury has caused impairment such as nerve or palm involvement in addition to the amputation, such impairment must be considered in the determination. The DMA will calculate the impairment of each digit separately and combine them for a total percentage of loss to the hand or foot. Where the cumulative allowances for the individual digits are greater than the percentage of loss for the entire hand or foot, the higher percentage should be used.
b. Loss of Hearing. After a complete report is received, the percentage of hearing loss is calculated using Form CA-51 (Exhibit 3). The DMA will then verify the calculation and the CE will certify the correctness of the DMA's computations. Adjudications based on just one audiogram should be avoided.
(1) Air vs. Bone Conduction. Air conduction studies provide a complete picture of how well an individual can actually hear, while bone conduction studies show what part of the hearing loss resulted from nerve damage. While it is not unusual for air conduction studies to show a greater hearing loss than bone conduction, the opposite results are medically inconsistent and render the audiogram useless. Therefore, while all audiograms must show test results for bone conduction and pure tone air conduction studies, a schedule award may not be based on the results of bone conduction studies.
(2) Computation. Effective February 24, 1986, hearing loss awards are based on the formula contained in the AMA Guides. (FECA Program Memoranda Nos. 162, 181, and 217 describe the previous frequencies and computation methods.) Awards are computed as follows:
(a) Monaural Loss. The average of decibel loss in the frequencies of 500, 1000, 2000 and 3000 cps should first be determined. From this amount 15 decibels should be subtracted if ASA calibration was used and 25 decibels if ISO-ANSI calibration was used. The result should be multiplied by a factor of 1.5 to determine the percentage of loss.
(b) Binaural Loss. The monaural loss for each ear should first be computed as described above. The percentage of loss in the better ear should then be multiplied by five and the result added to the percentage of loss in the worse ear. This sum should then be divided by six to determine the percentage of binaural loss. Percentages should not be rounded until the final percent for award purposes is obtained. Fractions should be rounded down from .49 or up from .50.
Between March 7, 1977 and February 23, 1986, the OWCP used only the frequencies of 1000, 2000, and 3000 cps to determine an award for hearing loss.
(3) Progression. Noise-induced hearing loss does not typically progress after exposure to noise ceases. A claim with an audiogram showing less than a 25 decibel loss soon after exposure ceases and a second audiogram showing a ratable loss may be denied if the DMA provides a well-reasoned opinion. Other benefits are still payable if any employment related hearing loss exists.
c. Loss of Vision. The percentage of impairment continues to be based on best uncorrected vision. See 5 U.S.C. 8107 (19). Loss of binocular vision or for loss of 80 percent or more is the same as for loss of the eye. See 5 U.S.C. 8107 (14).
d. Loss of Function of Bodily Organs. The FECA provides for award of compensation due to permanent impairment to the extremities and organs. However, most impairment ratings under the Sixth Edition of the AMA Guides evaluate impairment based on injury or disease. Therefore, special calculations are required to interpret certain ratings completed using the AMA Guides into figures usable under the Act.
(1) Lung Impairment. All claims involving impairment of the lungs where exposure occurred during Federal employment on or after September 7, 1974 (see Program Memorandum No. 269) will be evaluated for schedule award purposes. The class of respiratory impairment should first be established, following the AMA Guides as far as possible.
(a) While pulmonary function varies from day to day and from environment to environment, impairment exists for compensation purposes when the pulmonary function testing reveals Class 1 or greater impairment severity as defined by the AMA Guides.
(b) A Class 0 respiratory impairment equates to zero percent impairment of the whole person. An individual in this category would be considered to have no ratable loss and would not be entitled to compensation under the Act.
(c) Awards are based on the loss of use of both lungs, and the percentage for the particular class of whole person respiratory impairment will be multiplied by 312 weeks (twice the award for loss of function of one lung) to obtain the number of weeks payable.
(d) In cases of anatomical loss by traumatic injury or surgery, evaluation will also be based on loss of lung tissue (by weight or volume). If the percentage of loss using this method is higher than the percentage based on loss of respiratory function, the award shall be made on the basis of loss of lung tissue. Anatomical evaluations will be made only with regard to the injured lung and will be based on a 156-week maximum award for each lung. Anatomical loss awards can be made for both lungs if the injury caused loss in both, but each lung must be evaluated separately.
(2) Loss of Function of Other Organs. While the AMA Guides express the impairment of bodily organs in terms of the whole person due to a particular injury or medical condition, a schedule award under the FECA is based on the percentage of impairment of the particular organ.
(a) Whole person impairment measurements can be directly translated into organ ratings in the case of vital organs, such as the lungs, where the total impairment of the organ(s) produces 100% impairment of the whole person. When the maximum whole person rating of the organ is less than 100%, direct translation of the whole person measurement into a percentage of impairment to the organ is not valid. In these cases, to obtain the percentage of impairment to an organ corresponding to a given whole person impairment, the following mathematical ratio should be used:
|
(A) |
= |
(X) |
In this equation:
(A) = Actual whole person impairment of the claimant,
(B) = Maximum whole person impairment for the injury or condition of the organ, and
(X) = Organ rating to be determined.
For example, if the maximum whole person impairment for an injury or disease of an organ is 25% and the actual whole person impairment of the claimant is 10%, then:
|
10 |
= |
(X) |
|
(X) |
= |
1000 |
|
(X) |
= |
40% impairment of the organ |
(b) For certain schedule organs which have more than one physiologic function, the AMA Guides provide whole person impairment scores for each affected system within that organ. When calculating the impairment of these organs, the DMA must consider all affected organ systems as instructed in the AMA Guides.
In these cases, the maximum whole person impairment ascribed to the particular organ injury or condition (B) is obtained by combining the maximum levels for all functions using the Combined Values Chart in the current edition of the AMA Guides. The actual whole person impairment (A) is obtained by combining all functional impairments found using the Combined Values Chart in the Guides.
For example, a claimant with an injury to the penis has a Class 3 penile (sexual) whole person impairment amounting to 15%, and Class 2 urethral impairment of 10%. A 15% whole person impairment combined with a 10% whole person impairment results in a whole person impairment of 24%. The maximum whole person impairment for the sexual function is 15% and urethral function is 28%. Using the Combined Values Chart, this amounts to 39% total whole person impairment. Then:
|
24 |
= |
(X) |
|
(X) |
= |
2400 |
|
(X) |
= |
62% impairment of the penis |
(c) In addition to the loss of use, the statute compensates for loss of an organ. If there is total loss of a single paired organ (such as a kidney, breast, testicle or ovary), the schedule award is generally based on the loss of the organ. In this situation, it is immaterial whether the remaining organ compensates functionally for the loss.
Back to Chapter 3-0700 Table of Contents
5. Disfigurement. The FECA [§8107(c)(21)] provides for payment of compensation not to exceed $3500 for disfigurement of the face, head or neck which is likely to handicap the claimant in securing or maintaining employment. The DMA will be asked to review such claims and to evaluate the employee's disfigurement. If the DMA finds that maximum medical improvement has occurred, the DMA will review the photographs submitted along with the medical evidence of record. The concurrence of the Assistant District Director (ADD) or the District Director (DD) must be obtained. Following the file review, the DMA and ADD or DD will write a memorandum to the file which contains a complete description of the disfigurement. If the DMA does not find that maximum medical improvement has occurred, but has submitted a statement as to whether plastic surgery may improve the appearance and decrease the degree of disfigurement and the claimant is amenable, the DMA should include in his or her statement information concerning arrangements for treatment.
Back to Chapter 3-0700 Table of Contents
Exhibit 1: USE OF SIXTH EDITION OF AMA GUIDES
Effective May 1, 2009, OWCP began using the Sixth Edition of the AMA Guides. This edition is significantly different from previous editions. There are extensive changes affecting the calculations of schedule awards for FECA claimants.
The biggest adjustment from previous editions involves the rating of permanent impairment based on a specific diagnosis rather than the extremity or organ system. In previous editions an impairment rating may have included multiple diagnoses within an organ or extremity. Under the Sixth Edition most ratings will consider only the diagnosis with the most impact on the rated bodily region. In the Fifth Edition of the Guides impairment ratings relied heavily on loss of range of motion and strength in comparison to a paired extremity. The Sixth Edition only incorporates these findings as they relate to the specific diagnosis evaluated.
1. The Sixth Edition of the Guides implements a paradigm shift in the way impairment evaluations are conducted. The stated vision of the Sixth Edition is based on five axioms, including: (1) Adoption of terminology and conceptual framework of disablement outlined by the World Health Organization's (WHO's) International Classification of Functioning, Disability, and Health (ICF); (2) Becoming more diagnosis-based and basing the diagnoses in evidence; (3) Optimizing rater reliability through simplicity, ease of application, and following precedent; (4) Rating percentages are functionally based to the fullest extent possible; and (5) Stressing conceptual methodological congruity within and between organ rating systems.
2. The evaluation methodology used in the Sixth Edition substantially revises the methods used in previous editions. The Guides characterize the objective of the new methodology to be consistent, enhance relevancy, promote precision, and standardize the rating process. The foundation of the new methodology is the diagnosis-based grid used for each organ system and chapter. Evaluators will rate impairment according to the diagnosis representing the source of the most impairment in the given bodily region. If there is more than one ratable diagnosis in an affected extremity, the rater should combine all regional impairments for a final impairment at the extremity level.
Each diagnosis grid is divided into five classes of impairment severity, ranked from '0' (no impairment) to '4' (very severe). Within each class are five severity grades categorized 'A' through 'E' (default 'C') with corresponding impairment percentages.
Raters distinguish the level of severity using criteria separated into key factors and non-key factors. These criteria consist of: history of clinical presentation, physical examination or physical findings, clinical studies or objective test results, and functional history. In most organ systems or disease processes, clinical history is the key factor which will determine the impairment class. However, objective test results or physical findings may serve as the key factor in select organ system evaluations. The evaluator will adjust the severity grade based on the results of the remaining criteria. These adjustments cannot exceed the percentage of impairment within the range specified by the designated class.
3. The Sixth Edition of the AMA Guides consists of seventeen chapters, one less than the Fifth Edition. Two cardiovascular chapters in the Fifth Edition are consolidated into one chapter in the Sixth.
4. Musculoskeletal regions in the Sixth Edition of the Guides consist of the upper extremities (Chapter 15), lower extremities (Chapter 16), and the spine and pelvis (Chapter 17). The upper extremity is divided into four separate regions, including digits and hand, wrist, elbow, and shoulder. The lower extremity is divided into three regions consisting of foot and ankle, knee, and hip. The spine and pelvis is divided into four regions, including cervical, thoracic, and lumbar regions, and the pelvis, consisting of the ilium, ischium, pubis, sacrum and coccyx. Diagnosis classes for the upper and lower extremities are broken into the following categories: Soft tissue; muscle and tendon; ligament; and bone and joint. If impairment scores are calculated in whole person ratings, they should be adjusted to individual extremity or organ system percentages using conversion charts or rates.
5. Impairment to the upper or lower extremities that is caused by a spinal injury should be rated consistent with the article "Rating Spinal Nerve Extremity Impairment Using the Sixth Edition" in the July/August 2009 edition of The Guides Newsletter published by AMA. The Guides Newsletter article (July/August publication by the AMA) titled "Rating Spinal Nerve Extremity Impairment Using the Sixth Edition" is Exhibit 4 in this chapter, and has been reproduced with permission from the AMA.
6. The chapter on impairments due to pain (Chapter 3) has been updated. As with the Fifth Edition, the Sixth Edition allows for a maximum 3% impairment rating for non-specific pain that cannot be attributed to a condition addressed elsewhere in the Guides. According to Section 3.3b:
Patients' responses on functional assessment instruments will act as modifiers of the percentage impairment they are awarded, the awards will, in general, primarily reflect objective factors. This is in keeping with the general strategy of the Guides to consider PRI [Pain-related impairment] but to limit the amount of impairment that is awarded for subjective factors. In no circumstances should the PRIs developed using this chapter be considered as an add-on to impairment determinations based on the criteria listed in Chapters 4 to 17. In essence, the PRIs derived according to this chapter are determined in a stand-alone fashion.
7. Entrapment neuropathy of the upper extremities (e.g. carpal tunnel, cubital tunnel, etc.) (Section 15.4f) must be documented with nerve conduction velocity (NCV) testing in order to consider ratable impairment. If testing was not conducted or does not meet the criteria outlined by the Guides, no ratable impairment may be considered. Only pre-operative testing is used for rating impairment in this section. Optimal rating time following surgical intervention is between nine months and 2 years. When evaluating multiple simultaneous neuropathies, the first (or most impairing) is rated at 100%, the second is rated at 50%, and the third is rated at 0%. If there are more than three neuropathies, the neurology chapter should be used rather than Chapter 15.
8. The Guides stipulate only permanent impairment may be rated, and only after the claimant has reached a point of "maximum medical improvement" (MMI). The Guides do not afford the rating of future impairment. Impairment should not be rated permanent until sufficient time has passed for healing and recovery, which may vary substantially depending on the condition and the claimant's profile. The clinical findings must indicate that the medical condition is stabilized for the claimant to have reached MMI. The Guides define MMI as "a status where patients are as good as they are going to be from the medical and surgical treatment available to them."
In cases where a claimant declines surgery or other curative treatment, an MMI determination may still be reached. The evaluating physician should make a written note in the report discussing the appropriateness of the prescribed treatment and the basis of the claimant's declination. The physician should also indicate that the individual is at MMI in lieu of additional treatment.
Claimants not at MMI, but with potential for future progression of their disease, can be rated for permanent impairment on the current findings; MMI does not preclude the worsening of a condition that is expected with the passage of time or due to the aging process.
Back to Chapter 3-0700 Table of Contents
Exhibit 2: Percentage Table of Schedule Awards, Form CA-699
|
MEMBER |
|
01% |
02% |
03% |
04% |
05% |
10% |
15% |
20% |
|---|---|---|---|---|---|---|---|---|---|
|
Arm |
W |
3.12 |
6.24 |
9.36 |
12.48 |
15.60 |
31.20 |
46.80 |
62.40 |
|
D |
21.84 |
43.68 |
65.52 |
87.36 |
109.20 |
218.40 |
327.60 |
436.80 |
|
|
Leg |
W |
2.88 |
5.76 |
8.64 |
11.52 |
14.40 |
28.80 |
43.20 |
57.60 |
|
D |
20.16 |
40.32 |
60.48 |
80.64 |
100.80 |
201.60 |
302.40 |
403.20 |
|
|
Hand |
W |
2.44 |
4.88 |
7.32 |
9.76 |
12.20 |
24.40 |
36.60 |
48.80 |
|
D |
17.08 |
34.16 |
51.24 |
68.32 |
85.40 |
170.80 |
256.20 |
341.60 |
|
|
Foot/Penis |
W |
2.05 |
4.10 |
6.15 |
8.20 |
10.25 |
20.50 |
30.75 |
41.00 |
|
D |
14.35 |
28.70 |
43.05 |
57.40 |
71.75 |
143.50 |
215.25 |
287.00 |
|
|
Vulva/Vagina |
W |
2.05 |
4.10 |
6.15 |
8.20 |
10.25 |
20.50 |
30.75 |
41.00 |
|
D |
14.35 |
28.70 |
43.05 |
57.40 |
71.75 |
143.50 |
215.25 |
287.00 |
|
|
Larynx/ |
W |
1.60 |
3.20 |
4.80 |
6.40 |
8.00 |
16.00 |
24.00 |
32.00 |
|
D |
11.20 |
22.40 |
33.60 |
44.80 |
56.00 |
112.00 |
168.00 |
224.00 |
|
|
Eye |
W |
1.60 |
3.20 |
4.80 |
6.40 |
8.00 |
16.00 |
24.00 |
32.00 |
|
D |
11.20 |
22.40 |
33.60 |
44.80 |
56.00 |
112.00 |
168.00 |
224.00 |
|
|
Kidney/ |
W |
1.56 |
3.12 |
4.68 |
6.24 |
7.80 |
15.60 |
23.40 |
31.20 |
|
D |
10.92 |
21.84 |
32.76 |
43.68 |
54.60 |
109.20 |
163.80 |
218.40 |
|
|
Thumb |
W |
.75 |
1.50 |
2.25 |
3.00 |
3.75 |
7.50 |
11.25 |
15.00 |
|
D |
5.25 |
10.50 |
15.75 |
21.00 |
26.25 |
52.50 |
78.75 |
105.00 |
|
|
1st Finger |
W |
.46 |
.92 |
1.38 |
1.84 |
2.30 |
4.60 |
6.90 |
9.20 |
|
D |
3.22 |
6.44 |
9.66 |
12.88 |
16.10 |
32.20 |
48.30 |
64.40 |
|
|
Great Toe |
W |
.38 |
.76 |
1.14 |
1.52 |
1.90 |
3.80 |
5.70 |
7.60 |
|
D |
2.66 |
5.32 |
7.98 |
10.64 |
13.30 |
26.60 |
39.90 |
53.20 |
|
|
2nd Finger |
W |
.30 |
.60 |
.90 |
1.20 |
1.50 |
3.00 |
4.50 |
6.00 |
|
D |
2.10 |
4.20 |
6.30 |
8.40 |
10.50 |
21.00 |
31.50 |
42.00 |
|
|
3rd Finger |
W |
.25 |
.50 |
.75 |
1.00 |
1.25 |
2.50 |
3.75 |
5.00 |
|
D |
1.75 |
3.50 |
5.25 |
7.00 |
8.75 |
17.50 |
26.25 |
35.00 |
|
|
Toe other |
W |
.16 |
.32 |
.48 |
.64 |
.80 |
1.60 |
2.40 |
3.20 |
|
D |
1.12 |
2.24 |
3.36 |
4.48 |
5.60 |
11.20 |
16.80 |
22.40 |
|
|
4th Finger |
W |
.15 |
.30 |
.45 |
.60 |
.75 |
1.50 |
2.25 |
3.00 |
|
D |
1.05 |
2.10 |
3.15 |
4.20 |
5.25 |
10.50 |
15.75 |
21.00 |
|
|
Hearing |
W |
.52 |
1.04 |
1.56 |
2.08 |
2.60 |
5.20 |
7.80 |
10.40 |
|
D |
3.64 |
7.28 |
10.92 |
14.56 |
18.20 |
36.40 |
54.60 |
72.80 |
|
|
Testicle/ |
W |
.52 |
1.04 |
1.56 |
2.08 |
2.60 |
5.20 |
7.80 |
10.40 |
|
D |
3.64 |
7.28 |
10.92 |
14.56 |
18.20 |
36.40 |
54.60 |
72.80 |
|
|
Hearing |
W |
2.00 |
4.00 |
6.00 |
8.00 |
10.00 |
20.00 |
30.00 |
40.00 |
|
D |
14.00 |
28.00 |
42.00 |
56.00 |
70.00 |
140.00 |
210.00 |
280.00 |
* Includes Fallopian tube
(W = weeks; D = days)
|
MEMBER |
|
25% |
30% |
35% |
40% |
45% |
50% |
55% |
60% |
|---|---|---|---|---|---|---|---|---|---|
|
Arm |
W |
78.00 |
93.60 |
109.20 |
124.80 |
140.40 |
156.00 |
171.60 |
187.20 |
|
D |
546.00 |
655.20 |
764.40 |
873.60 |
982.80 |
1092.00 |
1201.20 |
1310.40 |
|
|
Leg |
W |
72.00 |
86.40 |
100.80 |
115.20 |
129.60 |
144.00 |
158.40 |
172.80 |
|
D |
504.00 |
604.80 |
705.60 |
806.40 |
907.20 |
1008.00 |
1108.80 |
1209.60 |
|
|
Hand |
W |
61.00 |
73.20 |
85.40 |
97.60 |
109.80 |
122.00 |
134.20 |
146.40 |
|
D |
427.00 |
512.40 |
597.80 |
683.20 |
768.60 |
854.00 |
939.40 |
1024.80 |
|
|
Foot/Penis |
W |
51.25 |
61.50 |
71.75 |
82.00 |
92.25 |
102.50 |
112.75 |
123.00 |
|
D |
358.75 |
430.50 |
502.25 |
574.00 |
645.75 |
717.50 |
789.25 |
861.00 |
|
|
Vulva/Vagina |
W |
51.25 |
61.50 |
71.75 |
82.00 |
92.25 |
102.50 |
112.75 |
123.00 |
|
D |
358.75 |
430.50 |
502.25 |
574.00 |
645.75 |
717.50 |
789.25 |
861.00 |
|
|
Larynx/ |
W |
40.00 |
48.00 |
56.00 |
64.00 |
72.00 |
80.00 |
88.00 |
96.00 |
|
D |
280.00 |
336.00 |
392.00 |
448.00 |
504.00 |
560.00 |
616.00 |
672.00 |
|
|
Eye |
W |
40.00 |
48.00 |
56.00 |
64.00 |
72.00 |
80.00 |
88.00 |
96.00 |
|
D |
280.00 |
336.00 |
392.00 |
448.00 |
504.00 |
560.00 |
616.00 |
672.00 |
|
|
Kidney/Lung |
W |
39.00 |
46.80 |
54.60 |
62.40 |
70.20 |
78.00 |
85.80 |
93.60 |
|
D |
273.00 |
327.60 |
382.20 |
36.80 |
491.40 |
546.00 |
600.60 |
655.20 |
|
|
Thumb |
W |
18.75 |
22.50 |
26.25 |
30.00 |
33.75 |
37.50 |
41.25 |
45.00 |
|
D |
131.25 |
157.50 |
183.75 |
210.00 |
236.25 |
262.50 |
288.75 |
315.00 |
|
|
1st Finger |
W |
11.50 |
13.80 |
16.10 |
18.40 |
20.70 |
23.00 |
25.30 |
27.60 |
|
D |
80.50 |
96.60 |
112.70 |
128.80 |
144.90 |
161.00 |
177.10 |
193.20 |
|
|
Great Toe |
W |
9.50 |
11.40 |
13.30 |
15.20 |
17.10 |
19.00 |
20.90 |
22.80 |
|
D |
66.50 |
79.80 |
93.101 |
106.40 |
119.70 |
133.00 |
146.30 |
159.60 |
|
|
2nd Finger |
W |
7.50 |
9.00 |
10.50 |
12.00 |
13.50 |
15.00 |
16.50 |
18.00 |
|
D |
52.50 |
63.00 |
73.50 |
84.00 |
94.50 |
105.00 |
115.50 |
26.00 |
|
|
3rd Finger |
W |
6.25 |
7.50 |
8.75 |
10.00 |
11.25 |
12.50 |
13.75 |
15.00 |
|
D |
43.75 |
52.50 |
61.25 |
70.00 |
78.75 |
87.50 |
96.25 |
105.00 |
|
|
Toe (No |
W |
4.00 |
4.8 |
5.60 |
6.40 |
7.20 |
8.00 |
8.80 |
9.60 |
|
D |
28.00 |
33.60 |
39.20 |
44.80 |
50.40 |
56.00 |
61.60 |
67.20 |
|
|
4th Finger |
W |
3.75 |
4.50 |
5.25 |
6.00 |
6.75 |
7.50 |
8.25 |
9.00 |
|
D |
26.25 |
31.50 |
36.75 |
42.00 |
47.25 |
52.50 |
57.75 |
63.00 |
|
|
Hearing |
W |
13.00 |
15.60 |
18.20 |
20.80 |
23.40 |
26.00 |
28.60 |
31.20 |
|
D |
91.00 |
109.20 |
127.40 |
145.60 |
163.80 |
182.00 |
200.20 |
218.40 |
|
|
Testicle/ |
W |
13.00 |
15.60 |
18.20 |
20.80 |
23.40 |
26.00 |
28.60 |
31.20 |
|
D |
91.00 |
109.20 |
127.40 |
145.60 |
163.80 |
182.00 |
200.20 |
218.40 |
|
|
Hearing |
W |
50.00 |
60.00 |
70.00 |
80.00 |
90.00 |
100.00 |
110.00 |
120.00 |
|
D |
350.00 |
420.00 |
490.00 |
560.00 |
630.00 |
700.00 |
770.00 |
840.00 |
* Includes Fallopian tube
(W = weeks; D = days)
|
MEMBER |
|
65% |
70% |
75% |
80% |
85% |
90% |
95% |
100% |
|---|---|---|---|---|---|---|---|---|---|
|
Arm |
W |
202.80 |
218.40 |
234.00 |
249.60 |
265.20 |
280.80 |
296.40 |
312.00 |
|
D |
1419.60 |
1528.80 |
1638.00 |
1747.20 |
1856.40 |
1965.60 |
2074.80 |
2184.00 |
|
|
Leg |
W |
187.20 |
201.60 |
216.00 |
230.40 |
244.80 |
259.20 |
273.60 |
288.00 |
|
D |
1310.40 |
1411.20 |
1512.00 |
1612.80 |
1713.60 |
1814.40 |
1915.20 |
2016.00 |
|
|
Hand |
W |
158.60 |
170.80 |
183.00 |
195.20 |
207.40 |
219.60 |
231.80 |
244.00 |
|
D |
1110.20 |
1195.60 |
1281.00 |
1366.40 |
1451.80 |
1537.20 |
1622.60 |
1708.00 |
|
|
Foot/ |
W |
133.25 |
143.50 |
153.75 |
164.00 |
174.25 |
184.50 |
194.75 |
205.00 |
|
D |
932.75 |
1004.50 |
1076.25 |
1148.00 |
1219.75 |
1291.50 |
1363.25 |
1435.00 |
|
|
Vulva/Vagina |
W |
133.25 |
143.50 |
153.75 |
164.00 |
174.25 |
184.50 |
194.75 |
205.00 |
|
D |
932.75 |
1004.50 |
1076.25 |
1148.00 |
1219.75 |
1291.50 |
1363.25 |
1435.00 |
|
|
Larynx/ |
W |
104.00 |
112.00 |
120.00 |
128.00 |
136.00 |
144.00 |
152.00 |
160.00 |
|
D |
728.00 |
784.00 |
840.00 |
896.00 |
952.00 |
1008.00 |
1064.00 |
1120.00 |
|
|
Eye |
W |
104.00 |
112.00 |
120.00 |
160.00 |
160.00 |
160.00 |
160.00 |
160.00 |
|
D |
728.00 |
784.00 |
840.00 |
1120.00 |
1120.00 |
1120.00 |
1120.00 |
1120.00 |
|
|
Kidney/ |
W |
101.40 |
109.20 |
117.00 |
124.80 |
132.60 |
140.40 |
148.20 |
156.00 |
|
D |
709.80 |
764.40 |
819.00 |
873.60 |
928.20 |
982.80 |
1037.40 |
1092.00 |
|
|
Thumb |
W |
48.75 |
52.50 |
56.25 |
60.00 |
63.75 |
67.50 |
71.25 |
75.00 |
|
D |
341.25 |
367.50 |
393.75 |
420.00 |
446.25 |
472.50 |
498.75 |
525.00 |
|
|
1st Finger |
W |
29.90 |
32.20 |
34.50 |
36.80 |
39.10 |
41.40 |
43.70 |
46.00 |
|
D |
209.30 |
225.40 |
241.50 |
257.60 |
273.70 |
289.80 |
305.90 |
322.00 |
|
|
Great Toe |
W |
24.70 |
26.60 |
28.50 |
30.40 |
32.30 |
34.20 |
36.10 |
38.00 |
|
D |
172.90 |
186.20 |
199.50 |
212.80 |
226.10 |
239.40 |
252.70 |
266.00 |
|
|
2nd Finger |
W |
19.50 |
21.00 |
22.50 |
24.00 |
25.50 |
27.00 |
28.50 |
30.00 |
|
D |
136.50 |
147.00 |
157.50 |
168.00 |
178.50 |
189.00 |
199.50 |
210.00 |
|
|
3rd Finger |
W |
16.25 |
17.50 |
18.75 |
20.00 |
21.25 |
22.50 |
23.75 |
25.00 |
|
D |
113.75 |
122.50 |
131.25 |
140.00 |
148.75 |
157.50 |
166.25 |
175.00 |
|
|
Toe (Not |
W |
10.40 |
11.20 |
12.00 |
12.80 |
13.60 |
14.40 |
15.20 |
16.00 |
|
D |
72.80 |
78.40 |
84.00 |
89.60 |
95.20 |
100.80 |
106.40 |
112.00 |
|
|
4th Finger |
W |
9.75 |
10.50 |
11.25 |
12.00 |
12.75 |
13.50 |
14.25 |
15.00 |
|
D |
68.25 |
73.50 |
78.75 |
84.00 |
89.25 |
94.50 |
99.75 |
105.00 |
|
|
Hearing |
W |
33.80 |
36.40 |
39.00 |
41.60 |
44.20 |
46.80 |
49.40 |
52.00 |
|
D |
236.60 |
254.80 |
273.00 |
291.00 |
309.40 |
327.60 |
345.80 |
364.00 |
|
|
Testicle/ |
W |
33.80 |
36.40 |
39.00 |
41.60 |
44.20 |
46.80 |
49.40 |
52.00 |
|
D |
236.60 |
254.80 |
273.00 |
291.00 |
309.40 |
327.60 |
345.80 |
364.00 |
|
|
Hearing |
W |
130.00 |
140.00 |
150.00 |
160.00 |
170.00 |
180.00 |
190.00 |
200.00 |
|
D |
910.00 |
980.00 |
1050.00 |
1120.00 |
1190.00 |
1260.00 |
1330.00 |
1400.00 |
Back to Chapter 3-0700 Table of Contents
Exhibit 3: Hearing Loss Medical Opinion, Form CA-51 (Link to Image)
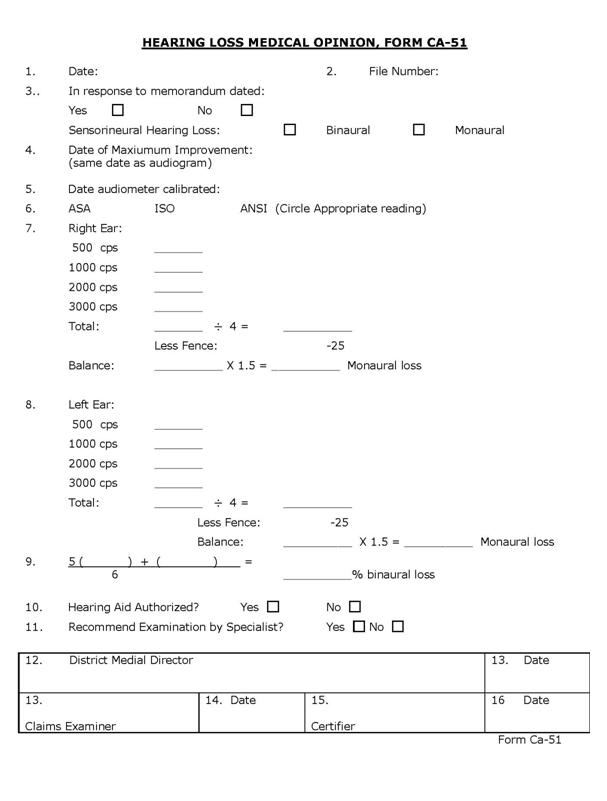
Back to Chapter 3-0700 Table of Contents
Exhibit 4: Use of Sixth Edition of AMA Guides (PLEASE CLICK THE IMAGE BELOW TO ACCESS THE FULL NEWSLETTER)
Back to Chapter 3-0700 Table of Contents
|
Paragraph and Subject |
Date |
Trans. No. |
|---|---|---|
|
Table of Contents |
05/94 |
94-24 |
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
Exhibits |
Date |
Trans. No. |
|---|---|---|
|
1. Procedures for Excluding Medical Providers (Link to Image) |
12/94 |
95-04 |
|
12/94 |
95-04 |
|
|
12/94 |
95-04 |
1. Purpose. Regulations appearing at 20 C.F.R. 10.450-457 furnish the basis for excluding medical providers, including physicians, hospitals, or suppliers of medical support services or appliances, from participation and payment under the FECA for fraud, abuse and other unacceptable practices. The regulations provide a mechanism for initiating and effecting exclusion while ensuring due process for medical providers. They also provide for reinstatement after specified time periods if reasonable assurance exists that the action which led to the exclusion will not recur. The purpose of this chapter is to describe the bases for exclusion and the procedures for excluding and reinstating medical providers. The procedures are shown in diagrammatic form in Exhibit 1 (Link to Image).
Back to Chapter 3-0800 Table of Contents
2. Extent of Sanctions. Excluded providers are not authorized to render services and OWCP will not pay their bills. Medical reports from an excluded physician may not be disregarded, but they may be accorded diminished probative value if the reason for exclusion warrants it. A memorandum should appear in the case file showing the reason for exclusion and the rationale for according diminished probative value to the report. The Claims Examiner (CE) should prepare the memorandum unless the reasons for exclusion or the extent to which the probative value is diminished require the expertise of the District Medical Adviser (DMA) to prepare it.
Back to Chapter 3-0800 Table of Contents
3. Automatic Exclusion. A provider is automatically excluded from participation under the FECA if he or she has been:
a. Convicted under any criminal statute for fraudulent activities in connection with any Federal or State program for which payments are made to providers for similar medical, surgical, or hospital appliances or supplies; or
b. Excluded or suspended, or has resigned in lieu of exclusion or suspension, from participation in such a program.
Most automatic exclusions will result from action by Medicare, which is administered by the Health Care Financing Administration (HCFA), but some will result from action by other Federal programs or by state Medicaid programs. (The grounds for exclusion under HCFA include sale and distribution of illegal drugs.) Providers convicted under any criminal statute for fraudulent activities in connection with any Federal or state program for which payments are made for medical services are also automatically excluded by OWCP. District offices should notify the National Office of any convicted providers who are not on the exclusion list. Since such convictions are sometimes overturned on appeal, the district office should not exclude providers under these procedures until documentation of the conviction is obtained by the National Office.
Back to Chapter 3-0800 Table of Contents
4. Non-Automatic Exclusion. Exclusion for reasons other than those noted above is not automatic and must be initiated in the district office. A provider is subject to exclusion for fraud or abuse if she/he has:
a. Knowingly made or caused to be made any false statement or misrepresentation of a material fact in connection with a determination of the right to reimbursement under the FECA, or in connection with a request for payment (20 C.F.R. 10.450(c)). This provision generally applies to billings for services or supplies which were never furnished.
(1) Unusually Frequent Billings. DMAs, CEs and Benefit Payment Clerks (BPCs) should be alert to instances of unusually frequent office visits or use of prescription drugs or supplies. In such instances the CE should write to the claimant and ask whether the services or supplies in question were actually received and, if so, why the claimant believes they were needed.
(2) Contacting Physicians. If the claimant states that some services or supplies were never furnished and the provider is a physician, the CE will refer the case to the DMA, who should write to the physician, describe the apparent false billing, and request an explanation within 30 days. The DMA should review any reply within the context of the case and prepare a memorandum to the Supervisory Claims Examiner (SCE) concerning possible violation of the regulations. If the physician does not reply within 30 days, the DMA should so advise the SCE.
(3) Contacting Non-Physicians. If the claimant states that some services or supplies were never furnished and the provider is not a physician, the CE will contact him or her to obtain an explanation. If the provider does not reply, or if the reply fails to establish that the billing in question was appropriate,S the CE should prepare a memorandum to the Assistant District Director as described in paragraph 9 (a)(1) of PM Chapter 2-402 for possible referral to the Office of the Inspector General.
b. Submitted, or caused to be submitted, three or more bills or requests for payment under the FECA within a twelve-month period containing charges which the Office finds are substantially in excess of the provider's customary charges, unless it is found that there is good cause for the bills or requests containing such charges (20 C.F.R. 450(d)).
(1) Reimbursement. A provider who charges more than the amount allowed by the fee schedule will not be penalized if the amount corresponds to the amount charged other patients. If the claimant has paid the full amount charged prior to notification that the excess is not payable, and then requests reimbursement, the provider will be asked to reimburse the claimant for the amount over and above the allowable fee or submit an explanation to OWCP for the additional charge. Failure of the provider to make such reimbursement within a reasonable time or to provide satisfactory justification will be deemed collection of a fee warranting initiation of the exclusion procedures.
(2) Notification. If the provider is charging FECA claimants a significantly higher price for identical services, appliances, or supplies, the DMA should write to the provider. The letter should state that the Office has found through investigation that it is being billed more than the customary charge for the specific service(s) and invite the provider to give the reason, if any, for the higher charges. The provider should also be advised that absent such reasons he or she should cease such practice or face possible exclusion.
(3) Response. If the provider replies that the extra charges are made because of special requirements of FECA cases, such as studying files or writing medical reports, he or she should be instructed to show the charge for reports and file review separately.
(4) Advice to RD. Serious or persistent occurrences of excessive billing should be reported to the District Director (DD), and the DMA or DD should telephone the provider to discuss the problem. If the provider fails to cooperate, documentation of the situation should be routed to the Regional Director (RD) for further action. The documentation should include detailed written accounts of all telephone conversations as well as copies of pertinent correspondence.
c. Knowingly failed to timely reimburse claimants for treatment, services, or supplies furnished under the FECA and paid by the Government (20 C.F.R. 10.450(e)).
(1) Dual Payment. If a claimant states that he or she paid for services or supplies which were also paid by the Office without subsequent reimbursement, the SCE should write a letter of warning to the provider, with a copy to the claimant. The letter should bring the dual payment to the provider's attention and ask him or her to reimburse the claimant without delay. The letter should quote the grounds for exclusion and state that initiation of exclusion proceedings will be considered if the claimant is not reimbursed within 30 days.
(2) Follow-up. The SCE or CE should contact the claimant 30 days after release of this letter to ensure that the claimant has received the reimbursement. If not, a copy of all material related to the complaint should be routed to the DD. Serious or persistent offenses should be referred to the RD for consideration of exclusion, and material on such providers should be maintained in the Provider Exclusion File.
d. Failed, neglected, or refused, on three or more occasions during a twelve-month period, to submit full and accurate medical reports, or to respond to requests by the Office for additional reports or information, as required by the FECA and by 20 C.F.R. 10.450 (f)).
(1) No Response. When a third request for a medical report must be made and a response is not received within a reasonable period, the CE will refer the case to the DMA. The DMA will telephone the provider and explain the problem, noting that failure to submit full and accurate reports or to respond to a reasonable request for further information may lead to exclusion from the program.
(2) Inadequate Response. The CE should also refer the case to the DMA when a medical report is incomplete and/or inaccurate and repeated requests for additional information have not received satisfactory response. The DMA should state whether the information is in fact incomplete or inaccurate, and if the request for additional reports or information is reasonable. If so, the DMA should telephone the provider as described above.
(3) Further Action. In intractable cases, the DMA should refer the matter to the DD, who will study the documentation and take further action as indicated, such as additional contact with the provider or referral to the RD for consideration of exclusion.
e. Knowingly furnished treatment, services, or supplies which are substantially in excess of the claimant's needs, or of a quality which fails to meet professionally recognized standards (20 C.F.R. 10.450 (g)).
(1) DMA Advice. CEs and BPCs may ask the DMA if services or supplies are substantially in excess of a claimant's needs or fail to meet professionally recognized standards. The DMA should place a memorandum in the file which addresses the issue and which contains medical rationale for the opinion. The DMA may also identify instances of excessive treatment, services, or supplies in the course of reviewing cases for other reasons. Any question regarding standards or quality should be referred to the DMA for advice and opinion.
(2) Contacting Physicians. The DMA will telephone a provider who is a physician and discuss the issue. If the discussion does not resolve the problem, the DMA will write a letter of warning to the provider which specifies the services or supplies and gives the reason why they are considered excessive or unacceptable and do not meet professionally recognized standards. The letter will also quote the exclusion provision of 20 C.F.R. 10.450 (g).
(3) Contacting Non-Physicians. The SCE will write a letter of warning to a provider who is not a physician, citing the regulations and explaining why the services or supplies are considered to be in violation of them.
(4) Referral to RD. If the DMA finds that a provider is engaging in a medical practice which is life- threatening or harmful, the DMA will refer the matter to the DD with all documentation for routing to the RD.
While non-automatic exclusion may be initiated for any of the practices indicated above, the right to exclude a provider should be exercised with restraint. Every effort should be made to correct unacceptable or deficient practices by letters and telephone calls before taking further action. The RD will initiate exclusion only when it becomes apparent that continued attempts to educate and persuade will not terminate unacceptable activities. Of course, it is not necessary or desirable to attempt to reform a provider who is engaging in harmful medical practices. In such cases exclusion should be undertaken without delay.
Back to Chapter 3-0800 Table of Contents
5. Formal Notification to Providers. It is essential that the district office act promptly after grounds for exclusion are discovered, since abuses must be curtailed without delay. Cases referred to the SCE and to typing for warning letters should receive priority queuing, and material forwarded to the RD for consideration of exclusion should be designated as "special" and treated as such during all processing in the RD's office.
a. Provider Exclusion File. The RD will maintain a Provider Exclusion File containing copies of evidence, memoranda and letters to reflect action taken by the district office in each instance of alleged fraud or abuse. When such material is routed to the RD, he or she will review it along with any other material in the file on the same provider.
b. Preliminary Steps. The RD will obtain whatever additional information he or she may deem appropriate and will try to resolve the problem without issuing a letter of intent to exclude. The RD will ensure that thorough and reasonable steps were taken by district office staff to curtail unacceptable provider practices. If feasible, the RD may suggest that a meeting be arranged with the provider and the DMA present in order to achieve compliance. If the provider is amenable to a conference call, it should be arranged.
c. Consultation with Solicitor and National Office. If reasonable educational and persuasive efforts have proven futile, or in the event of a harmful or life-threatening medical practice, the RD should discuss the situation with the Regional Office of the Solicitor. Prior to drafting a letter of intent to exclude, the RD shall telephone the Director for FEC to apprise him or her of the proposed action and the reasons for it. A sample letter of intent meeting the requirements of 20 C.F.R. 10.452 is shown as Exhibit 2.
d. Letter of Intent. The RD may issue a letter of intent to exclude if the provider has engaged in an unacceptable practice in violation of 20 C.F.R. 10.450 (c), (e) or (g). The RD may also issue a letter of intent to exclude for violation of 20 C.F.R. 10.450 (d) or (f) if there have been three instances of violation of either subsection (d) or (f) within any continuous twelve-month period. The instances of excessive charges or deficient reports may have occurred in the same or different cases.
(1) Excessive Charges. In order to be counted as an offense toward violation of 20 C.F.R. 10.450 (d), the excessive charges must be for services or supplies furnished on different dates, not duplicate billings for the same goods or service. Each excessive billing for a service or supply which is furnished on different occasions would constitute a separate and distinct occurrence which should be counted individually. For example, excessive charges for each of three office visits within a continuous twelve-month period will be grounds for exclusion.
(2) Inadequate Reports. Each instance of failure, neglect or refusal to submit a full and accurate medical report in response to a specific request by the district office, or to respond to a request for additional information, will be considered as one offense toward violation of 20 C.F.R. 10.450 (f). An initial inadequate report which is not submitted in response to a specific request from the Office will not count as an offense.
(3) Cumulative Occurrences. The regulations specify three instances of excessive charges or three instances of deficiencies in reports as separate grounds for exclusion. Therefore, two instances of one and one instance of the other will not constitute a basis for exclusion.
e. Information to Provider. The letter to the provider must be sent by certified mail, return receipt requested. Copies of supporting evidence such as deficient medical reports and documentation of billing improprieties may be attached as appropriate. The RD will maintain a five week call-up for the provider's response. A copy of the letter of intent and appropriate documentation should be sent to the Director for FEC.
Back to Chapter 3-0800 Table of Contents
6. Procedures for Exclusion. The RD will ensure that the provider has a full 30 days to reply to the letter of intent before taking further action.
a. Provider Response.
(1) No Response. If the provider fails to give written response within 30 calendar days, the RD will issue a decision to exclude as described below.
(2) Resignation. If the provider responds by submitting a letter of resignation, the RD will so inform the Director for FEC by telephone and follow up with a brief memorandum giving the provider's name, address and Tax Identification Number (TIN). The reinstatement provisions at 10.457(a) do not apply to those who resign. The RD should therefore write to the provider simply to acknowledge receipt of the resignation. If the provider resigns verbally, the RD should send him or her a letter confirming the resignation for his or her signature and allow 30 days for return of the signed resignation.
(3) Additional Evidence. If the provider responds within 30 calendar days with a request for consideration of additional evidence, the RD will carefully study all the evidence and decide whether or not the provider should be excluded. The RD should maintain liaison with the Solicitor's Office and should keep the Associate Director informed by telephone of the contents of any reply and its effect on the decision.
b. Issuing the Decision.
(1) Contents. The RD will send a letter decision stating the reasons for exclusion to the provider by certified mail, return receipt requested. If no reply was received to the letter of intent, it may be incorporated by reference. If further information was submitted, it must be evaluated in relation to the violations which prompted the letter of intent. The decision must also include the period of exclusion, an explanation of the reinstatement process and the provider's rights to further review of the exclusion. A copy of the decision should be sent to the Director for FEC. A sample decision is shown in Exhibit 3.
(2) Request for Hearing. A decision to exclude takes effect 30 calendar days from the date of the decision. During this period, the provider may file a request for a hearing before an Administrative Law Judge (ALJ) by addressing such request to the RD. The filing of a request for hearing within the 30 calendar day period stays the decision to exclude. Therefore, flagging of the automated provider file and notification of other parties must be held for 30 calendar days pending a request for a hearing.
(3) Further Action. If no request for a hearing is received within 30 calendar days following the RD's letter of decision, the RD shall so notify the Director for FEC in writing. The National Office will add the provider's name to the list of excluded providers distributed to all district offices and will notify state and local licensing agencies.
c. Requests for Hearing.
(1) Forwarding the Request. If a request for a hearing is received within 30 calendar days, the RD will send it to the Office of Administrative Law Judges, U.S. Department of Labor, 200 Constitution Avenue, N.W., Washington, D.C. 20210. A copy will be retained in the Provider Exclusion File.
(2) Copies of Request. A copy of the request for hearing will be sent to the Regional Solicitor, with a copy of all information concerning the provider from the Provider Exclusion File. Another copy of the request for hearing will be sent to the Director for FEC.
(3) Late Requests. If a request for a hearing is received later than 30 calendar days from the decision, the RD will advise the provider that it was not timely filed and that the request cannot be honored. A copy of this letter should be sent to the Director for FEC.
(4) ALJ Decision. The decision of the ALJ is effective on the date issued. An ALJ decision affirming exclusion can be stayed only by order of the Director, upon petition for review filed for grounds specified at 20 C.F.R. 10.455(c). Review by the Director is a matter of discretion rather than right. Upon notification of an ALJ's decision affirming exclusion, the district office and National Office will effect the exclusion by notifying interested parties and implementing stop payment flags and related procedures as described below.
d. Reinstatement of an Excluded Provider. An excluded provider may be reinstated after specified time periods, but only when reasonable assurances exist that the basis for the exclusion will not be repeated. Reinstatement is considered in the National Office and each district office will be advised of any reinstated providers.
Back to Chapter 3-0800 Table of Contents
7. Documentation and Advice to Affected Claimants. The National Office periodically publishes lists of excluded and reinstated providers which are organized by state and distributed to district offices.
a. List of Excluded Providers. Upon receiving the list, the district office should detach and reproduce the section of the list covering physicians within its jurisdiction and distribute it to local Federal agencies. The district office should also compare the list to its Provider Master File to identify any excluded providers who are treating claimants. For any excluded provider identified, the district office will run a Provider Utilization Report without awaiting receipt of the next general list.
b. Notification to Claimant. Form CA-1342 should be sent to each claimant seen by the provider within the past six months. The letter will inform the claimant that the provider has been excluded from furnishing medical services, supplies or appliances under the FECA and that any charges incurred more than 15 days after the date of the letter will not be paid. If the excluded provider is a physician, the claimant will be asked to select another physician and advised that he or she will be responsible for all charges incurred if treatment with the excluded physician is continued.
c. Removal from Roster. The Medical Management Assistant (MMA) will delete the excluded provider, if a physician, from the roster of second opinion and referee physicians. If an examination with the excluded physician is pending, the MMA will cancel the appointment and arrange to have the claimant examined by another specialist. If the excluded physician has been following a claimant after referral by the Office, care should be transferred to another physician.
d. Claimant Responses. If a claimant who is using the services of an excluded provider asks that the provider continue to be authorized to render services in his or her case and/or that the Office continue to pay for such services, the CE should explain as tactfully as possible the reason the provider has been excluded and why it is in the best interests of the claimant and the Office to use another provider.
e. Formal Decisions. If the claimant persists in submitting bills from the excluded provider, a compensation order should be issued rejecting the claim for services, supplies or appliances furnished by the provider for the reason that the provider has been excluded under 20 C.F.R. 10.450. As in any other adverse decision, the denial should be accompanied by the rights to hearing, reconsideration and appeal.
Back to Chapter 3-0800 Table of Contents
Exhibit 1: Procedures for Excluding Medical Providers (Link to Image)
Back to Chapter 3-0800 Table of Contents
Exhibit 2: Sample Letter of Intent To Exclude
Dear NAME OF RECIPIENT:
I am writing to inform you that it is my intention to exclude [you, and/or name of hospital, firm, etc.] from payment and participation as a provider of medical services, medical support services, and/or supplies to injured Federal employees under the Federal Employees' Compensation Act.
This action will be taken because [concisely state the grounds and cite the C.F.R. section, e.g. "you submitted three bills in a twelve month period substantially exceeding your customary charges for these services without good cause, a violation of 20 C.F.R. 10.450(d)." Then summarize the information you relied upon and refer to supporting documentation which will be attached].
Please telephone me at TELEPHONE NUMBER if you wish to inspect the record or obtain copies of any documentation not attached.
If you do not contest this action, you may resign voluntarily from participation in the FECA program without admitting or denying the above-stated grounds for exclusion.
If you do not choose to resign, you may request a decision on exclusion based upon the existing record and any additional documentary information you may wish to provide. You will have the right to request a formal hearing on any adverse decision before an Administrative Law Judge.
Your answer must be received by the undersigned within 30 days. You must state whether (a) you are resigning voluntarily or (b) you are requesting a determination on the existing record and any additional information you are providing. If you chose option (b), the additional information, if any, must be enclosed with your reply.
If you do not reply within 30 days of your receipt of this letter, it will be assumed that the allegations contained above are true, and you will be excluded from the FECA program as proposed.
Sincerely,
REGIONAL DIRECTOR
Back to Chapter 3-0800 Table of Contents
Exhibit 3: Sample Decision To Exclude
Dear NAME OF RECIPIENT:
Inasmuch as you have not responded to my letter of DATE, wherein I proposed to exclude you as a provider of [medical services, medical support services, supplies] under the Federal Employees' Compensation Act, the allegations stated in that letter are deemed to be true and are hereby incorporated as a part of this letter decision.
OR
I have carefully reviewed the information you submitted in response to my letter dated DATE, wherein I proposed to exclude you as a provider of (medical services, medical support services, supplies) under the Federal Employees' Compensation Act. [Include discussion of findings.]
Based upon these findings, NAME OF PROVIDER is hereby excluded from participation and payment as a provider under the Federal Employees' Compensation Act, for violation of 20 C.F.R. 10.450 [specify c, d, e, f and/or g, whichever applies]. This exclusion is effective 30 days from the date of this letter and shall last for a period of STATE PERIOD.
You may, of course, continue to provide services or supplies for the effects of injuries and occupational diseases under the Federal Employees' Compensation Act, if permitted by your State and local licensing agencies. However, payment is the responsibility of the patient or consumer and will not be reimbursed by this Office.
You may request a hearing on this decision by writing to the undersigned within 30 days of this letter. If such request is timely filed, the decision to exclude will be stayed. No hearing will be scheduled if the request is received after 30 days. Your timely request will be forwarded to the Department's Chief Administrative Law Judge for assignment.
A request for a hearing should contain (1) a concise notice of the issues on which you desire to give evidence at the hearing, (2) any request for a more definite statement by this Office, (3) any request for the presentation of oral argument or evidence, and (4) any request for a certification of questions concerning professional medical standards, medical ethics or medical regulation for an advisory opinion from a competent recognized professional organization or Federal, State or local regulatory body.
Reinstatement after exclusion is not automatic. You may request reinstatement as a provider after the period of exclusion has expired, or after one year, whichever occurs first. Any request for reinstatement should be addressed to the Director for Federal Employees' Compensation, U.S. Department of Labor, Office of Workers' Compensation Programs, 200 Constitution Avenue, N.W., Room S-3229, Washington, D.C. 20210.
The application for reinstatement should contain a concise statement of the basis for any application and should be accompanied by supporting documents and affidavits. The request for reinstatement may include a request for oral argument, but such argument will be allowed only in unusual circumstances where it will materially aid the decision-making process. The Director will order reinstatement only in instances where such reinstatement is clearly consistent with the ultimate goal of the regulations under which this action is taken, to protect the FECA program against fraud and abuse. To satisfy this requirement, the provider must furnish reasonable assurances that the basis for the exclusion will not be repeated.
Sincerely,
REGIONAL DIRECTOR
Back to Chapter 3-0800 Table of Contents
|
Paragraph and Subject |
Date |
Trans. No. |
|---|---|---|
|
Table of Contents |
11/98 |
99-06 |
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
10/90 |
91-02 |
|
|
7. Effect of Claims Actions on Entitlement to Medical Benefits |
10/90 |
91-02 |
|
11/98 |
99-06 |
|
Exhibits |
Date |
Trans. No. |
|---|---|---|
|
1. Sample Recruitment Letter and Reply—Second Opinion Examiner |
12/94 |
95-04 |
|
12/94 |
95-04 |
|
|
3. General Information for Physicians, Form CA-21 (Link to Image) Pages 1-2 |
12/95 |
95-04 |
|
12/94 |
95-04 |
|
|
12/94 |
95-04 |
1. Purpose. The work of the Medical Unit includes administrative as well as medical aspects. The purpose of this chapter is to describe these administrative considerations and procedures.
Back to Chapter 3-0900 Table of Contents
2. Obtaining Outside Medical Services. Federal regulations determine the method of compiling the roster of physicians from whom second opinion specialists and case reviewers will be selected. The requirements include public notice or other recruitment methods to advertise OWCP's need for and willingness to purchase certain medical consultation services; broad methods of distribution so that every qualified provider who wishes to participate has an opportunity to do so; and written agreements specifying the nature of services to be performed and the terms of purchase, so that the provider may be held accountable for any failure to provide the service as promised.
a. Recruitment. District offices may use various methods of recruitment, including:
(1) Writing or telephoning physicians listed in national or local rosters of medical specialists.
(2) Contacting officers of local medical and hospital associations, departmental chairpersons of medical schools, hospital staffs, and other government agencies which employ physicians. The letters shown in Exhibits 1 and 2 may be used for this purpose.
(3) Advertising through county medical societies or through publications of other organizations.
The District Medical Director (DMD) is responsible for conducting the district office's outreach function (see Chapter 3-200.3). Form CA-21 (Exhibit 3 (Link to Image)) may be used to provide prospective consultants with general information concerning their role and the program.
b. Insufficient Number of Physicians. If too few physicians respond to recruitment efforts, the list may be expanded by drawing on other sources. For example, the DMD may call or write physicians known to be available in the area on a case-by-case basis. As long as all qualified physicians who express willingness to examine claimants or perform case reviews receive an equitable share of referrals, the Office may freely use other physicians who did not respond to the recruitment or advertisement. Where specialists are scarce, second opinion examiners or case reviewers need not be Board-certified or Board-eligible.
c. Acceptability. The DMD should provide information to the District Director (DD) about the responsiveness and professional qualifications of physicians who apply to provide services and about an appropriate range of fees. The contracting officer (or designee) should interview each physician by telephone or in person to fix a reasonable cost or range of fees per service, and to establish a method whereby the physician will obtain referrals. Physicians who will review case files may obtain them by mail or in person from the district office. The contracting officer should avoid committing the Office to a minimum number of referrals to any one physician. The DMD should, however, be able to provide a verbal estimate of the workload.
If a physician with a demonstrably poor record of timeliness, responsiveness, or completeness of reports asks to provide service, the DMD should contact the physician and explain the program and its requirements, stressing the need for promptness, the standards for reports and the importance of responsiveness to questions. If interest continues, the physician may be asked for an opinion on one or two cases prior to contracting so that his or her understanding of the program and the kinds of issues on which opinions are needed may be demonstrated. Physicians may be advised that the reports are insufficient for the Office's needs, or that the Office has a sufficient number of specialists for present workloads. The district office should, however, avoid writing extensively critical letters to physicians.
d. Written Agreements. All physicians who regularly review cases for the Office should be placed under written agreement. Physicians who complete such agreements should not be asked to perform referee examinations while the contract is in force, and office records should be annotated to show the physicians in this category.
The contracting officer within each region is the Regional Director (RD), who is responsible for ensuring that they procedures are followed. The authority to sign agreements with physicians may be delegated in writing to the DD, but no further delegation is permitted. Sample agreements are shown in Exhibits 4 and 5.
e. Record-Keeping. The Medical Management Assistant (MMA) should maintain careful records in order to demonstrate compliance with these procedures. The following should be documented:
(1) Recruitment efforts and responses to them;
(2) Use of each physician responding, or reasons for not doing so;
(3) Contractual agreements with all physicians serving as case reviewers.
Back to Chapter 3-0900 Table of Contents
3. Release of Medical Information. While Federal regulations require the Office to maintain the confidentiality of records under its jurisdiction, they also provide that the claimant may have access to records pertaining to him or her as long as the information released will not be harmful. In most instances the regulations prohibit release of information to others unless the claimant has given written permission to release the records.
a. Release by OWCP. With written consent from the employee, the CE may release medical records to the representative, a private insurance company, a welfare agency, etc. If the CE believes that information contained in the records may be embarrassing or damaging to the claimant, the case will be referred to the DMA for review to determine whether release is advisable. Extreme caution should always be exercised when considering release to any party of medical information containing diagnoses or impressions of sexual deviation, drug addiction, alcoholism, psychotic conditions, or conditions resulting from self-abuse. The DMA may suggest release to the employee's treating physician for interpretation.
(1) Claimant or Representative. The DMA may be asked to render an opinion whether release of medical records would have an adverse effect upon the claimant. If so, the information will normally be released only to the employee's physician for interpretation.
(2) Claimant's Physician. When the claimant's attending physician wishes to study x-rays, electrocardiograms, slides, etc., made by another physician, clinic, or hospital, it is proper to authorize such review. These materials may be sent to the requesting physician by certified mail with the understanding that measures will be taken to avoid loss in transit and to return the materials promptly.
(3) Medical Departments of Other Federal Establishments. It is customary to furnish copies of medical reports of authorized examinations in connection with an injury to medical departments of other Federal establishments upon request.
(4) Office of Personnel Management (OPM). Medical information, usually in the form of copies of pertinent medical records, may be furnished the Office of Personnel Management upon request.
(5) Social Security Administration. Medical information, usually in the form of copies of pertinent medical reports, may be furnished the Social Security Administration upon request.
(6) Attorneys in Third Party Cases. All requests for medical information on third party cases shall be referred to the CE designated to handle such cases.
(7) Insurance Companies. Information may be released to an insurance company when the request is accompanied by a signed release from the employee.
Reports containing confidential information gathered by such agencies as the Federal Bureau of Investigation and the Office of the Inspector General remain the property of those agencies. Neither the reports nor communications concerning them may be disclosed outside OWCP without prior approval. Requests for access or disclosure of such reports or communications should be referred to the agency which generated the report.
Similarly, OWCP should not release reports labeled confidential by their authors. The requestor should be advised to contact the originator of such a report concerning its release.
b. Release of Medical Information by Others. The CE and DMA may be consulted by employing agencies, medical providers and others concerning the propriety of release of information pertaining to FECA claims. The following guidelines pertain to release of such information by parties other than OWCP:
(1) Medical Providers. Physicians providing medical services on OWCP authorization may release medical information to the claimant and his or her representative without OWCP approval, but they may not release such material to other parties, and they are not permitted to use such information for teaching purposes or to abstract it for publication without the specific approval of OWCP. If such release has occurred, the DMA should contact the physician and advise him or her that medical records pertaining to OWCP beneficiaries are privileged and confidential and may not be released to others without the specific approval of OWCP.
(2) Employing Agencies. The regulations state that all records, statements, and reports made in connection with a claim for compensation are the official records of OWCP and are not records of the agency, establishment, or department making or having the care or use of such records. Information needed for the official purposes of any department, agency, or other establishment of the Government may be disclosed if the employing agency certifies that such information will be used exclusively for official purposes.
(3) Federal Facilities. Federal hospitals and clinics may release medical information relating to OWCP beneficiaries from their records to medical officers of other Federal establishments without OWCP approval when requested for assistance in job placement or follow-up medical services. They may also release clinical information without OWCP approval to physicians for their assistance in caring for the patient. In general, Federal medical facilities may release medical information consistent with their responsibilities to safeguard the privacy of employees and protect sensitive information.
Any correspondence concerning medical care and related subjects will be prepared for the signature of the DMA where the district office has a full-time DMA. If the office has only a WAE (when actually employed) physician, correspondence will be prepared for the signature of that physician. The WAE physician will sign the correspondence or may designate the MMA to sign it using the physician's name.
Back to Chapter 3-0900 Table of Contents
4. Complaints Concerning Medical Care. The DMA may be asked to comment on complaints about the quality of medical care or about medical bias or discrimination. Complaints may range from minor matters such as prolonged waiting periods prior to examination by a particular physician to more serious problems which may potentially lead to malpractice or assault and battery suits. The CE is responsible for answering such complaints, but the DMA's professional expertise may be needed to prepare the response. Complaints Concerning Medical Care:
a. Medical Management. If a question arises concerning the attending physician's medical management of the case, the DMA should request discussion of the medical problem involved.
b. Guidelines for Attending Physician. In response to a complaint, the DMA may wish to seek consultation with experts in specialized fields in order to provide the attending physician with guidelines or to determine a further course of action with regard to medical care. In taking this action, the DMA should not mention any possible transfer of care to the specialist at a later date. Otherwise, the implication of bias may arise. The attending physician must be advised of the contemplated action and told that the findings will be made available to him or her.
Exclusion of medical providers is discussed in Chapter 3-800, while transfer of care to another physician is addressed in Chapter 3-300.
Back to Chapter 3-0900 Table of Contents
5. Fees for Medical Services. The Office maintains a fee schedule for certain medical services and supplies. The amounts payable are determined by assigning a value to each procedure which represents the relative skill, risk, and time required to perform it and according to whether it is medical, surgical, pathological, or radiological. Each value is then multiplied by a geographical index figure which represents the cost of medical care in the locality where the service is provided. Not all services are covered by the fee schedule, however, and if charges for a service which is not included appear to be unreasonable, the CE or Benefit Payment Clerk (BPC) may refer the case to the DMA for advice.
a. Determining Reasonableness. If the DMA cannot justify the charges on the basis of medical complications or other complexities of the case, either from information of record or through correspondence with the physician, the DMA should consult the local medical society for assistance in assessing the reasonableness of the charges. Fees higher than those charged the general public in the area for similar services will not be allowed without written justification in the case record and may be grounds for excluding the provider (see Chapter 3-800).
b. Services Not Rendered. Payment of medical expenses is made on the basis of services rendered. The law makes no provision for payment of services not rendered or for missed appointments except where OWCP scheduled the appointment. Payment may, however, be made to a physician for review of a file and preparation of a report.
c. Lost Wages. An employee who loses wages in undergoing examination or treatment authorized by OWCP may be reimbursed for these wages. The employee must submit a statement certified by the employer which shows the exact period of time and the total amount of wages lost. The statement must also furnish information needed to compute the amount of wages lost, such as rate of pay per hour or per day. Lost wages are paid only for the time needed for examination or treatment and travel needed to obtain it.
Back to Chapter 3-0900 Table of Contents
6. Case Maintenance and Handling.
a. Telephone Conversations and Personal Interviews. A written memorandum which provides a brief resume of the discussion must be prepared with respect to all substantive telephone conversations and personal interviews relating to OWCP claims (though not for brief, simple responses consisting of information about the program or the claim). Form CA-110, Report of Telephone or Office Call, may be used for this purpose. This does not apply to informal discussions with other members of the OWCP staff.
b. Memoranda and Notations by DMA. Material for inclusion in case files will be carefully worded in order to prevent any appearance of bias. Typed memorandums must bear the full signature of the DMA in red ink, unless the MMA signs for the DMA. The DMA's handwritten memorandum and notation will also be signed with red ink.
c. Underscoring. Annotation of medical reports contained in the case file is not permitted as it improperly focuses attention on certain parts of the report at the expense of others and may result in bias. Where the DMA feels such emphasis is necessary, he or she should prepare a memorandum for the file.
d. Order of Pages. Any pages removed for photocopying or other reasons should be replaced in the file in the sequence found. The order of documents numbered for the Employees' Compensation Appeals Board should not be disturbed.
e. Mailing of Case Records. The Branch of Records and Files is responsible for mailing the contents of case files from OWCP. They are to be sent by certified mail.
f. X-rays, Electrocardiograms, and Slides. Reports of x-ray and other kinds of tests are usually sufficient for determining medical issues, and it is rarely necessary to obtain the actual films, tracings, etc. Occasionally, however, the DMA may need to obtain such evidence for proper evaluation of the case. If so, it must be sent and returned by certified mail. All x-rays received in OWCP will promptly be referred to the DMA and returned to the sender as soon as they have served their purpose. If the sender cannot be identified, the x-ray will be referred to the present or latest attending physician and the injured employee notified.
Back to Chapter 3-0900 Table of Contents
7. Effect of Claims Actions on Entitlement to Medical Benefits.
a. Lump Sum Settlement. The receipt of a lump sum settlement for disability does not bar the claimant from receiving medical examination and treatment at OWCP expense.
b. Third Party Cases. An employee who has made a recovery from a third party is not entitled to treatment at OWCP expense until the remaining credit has been exhausted. Prior to authorizing medical care in such cases, the MMA should check with the designated CE to ensure that the OWCP will pay further medical expenses. When the Office of the Solicitor advises that a court hearing is imminent, all action must be held in abeyance pending the outcome of the suit. If a dire medical emergency exists, the Director for FEC should be contacted for instructions.
Back to Chapter 3-0900 Table of Contents
8. Time Loss for Routine Medical Appointments. As a rule, no more than four hours of compensation or continuation of pay should be allowed for routine medical appointments. Longer periods of time may be allowed when required by the nature of the medical procedure and/or the need to travel a substantial distance to obtain the medical care.
Back to Chapter 3-0900 Table of Contents
Exhibit 1: Sample Recruitment Letter and Reply—Second Opinion Examiner
Dear NAME OF PHYSICIAN:
The Federal Employees' Compensation Program is seeking physicians in your area to perform medical evaluations of Federal employees with traumatic injuries or occupational diseases.
As you may know, our program is responsible for providing medical and salary replacement benefits for Federal workers found to have work-related injuries or diseases. It is a non-adversarial system which relies on the medical community, not only for the treatment of our claimants, but also for the evaluation of the medical aspects of our cases. Medical evaluations are used by our claims examiners to adjudicate compensation claims properly and to manage them effectively.
A second opinion evaluation involves the physical examination of the worker, the review of the claim file and the submission of a written medical report answering specific questions posed by the claims examiner. In the report, you will be asked to give your opinion on issues such as the etiology of the condition and its relationship to the workplace, treatment, prognosis, and the assessment of any resulting physical impairment.
The program reimburses these services in full and, because these bills are subject to prompt pay rules, we are committed to process your bill within a short period of time.
Should you be interested in providing these services, please complete and mail the enclosed form. If you desire additional information or have any questions or comments regarding these services, please do not hesitate to call NAME on PHONE NUMBER.
Sincerely,
REGIONAL DIRECTOR
Dear REGIONAL DIRECTOR:
I would like to perform medical evaluations for the Federal Employees' Compensation Program. I am Board eligible ( ), Board certified ( ) in .
Sincerely,
(Signature)
(Print Name)
|
Office address(es) |
|
|
|
|
|
|
|
|
Office telephone number(s) |
|
|
|
|
|
Tax identification number |
|
Back to Chapter 3-0900 Table of Contents
Exhibit 2: Sample Follow-Up Letter—Second Opinion Examiner
Dear NAME OF PHYSICIAN:
Thank you for agreeing to perform medical evaluations for the Federal Employees' Compensation Program.
Please find below some details about our program, its requirements and claims processing system which may be of help to you and your office staff.
A. SCHEDULING
1. A member of our district office staff will call your office to arrange the second opinion examination. Generally, we prefer the actual examination to take place within 15 business days of this initial notification. If the claimant does not keep the appointment, please notify us at once.
2. We rotate medical evaluations among the physicians in the area who agree to perform these services. For this reason, some time may elapse between referrals.
B. BILLING
1. The program reimburses second opinion examinations in full. According to your billing practices, this may include your usual fee for a consultation as well as the time spent in reviewing the claimant's medical file, and any clerical time spent in typing the report. You may wish to itemize these charges in the bill.
2. Our prompt pay rules require that your bill be processed within 30 days. To ensure that your bill is indeed processed within this period of time, please be certain to use the billing form (HCFA-1500) enclosed with the case file. If this form is not used, we may have difficulty identifying your bill as one subject to the prompt pay rules and reimbursement may be delayed.
C. CLAIMANT'S FILE
1. You will receive photocopies of pertinent material from the original case file. These need not be returned to the district office.
2. Our files are arranged in chronological order, with the most recent material at the top of the file. If you need to remove a page from the spindle in order to examine it, please be sure to replace it where originally found. Also, please refrain from making notes in the margins of the reports and underlining any material in the file. We will try to identify the medical material for your attention.
D. MEDICAL REPORT
1. A complete medical report should be submitted to our district office within 15 business days of the actual second opinion examination.
2. The medical report should contain a brief synopsis of the clinical history of the claimant, a description of the physical findings and, most importantly, complete answers to all specific questions posed by the claims examiner. Should you find any question unclear as to wording or purpose, please contact our district office for clarification before answering the particular question. This may minimize the need for additional correspondence from the claims examiner.
3. Answers to the claims examiner's questions, particularly in the areas of etiology and work-relatedness, should be accompanied by an explanation or "rationale"; unsupported, brief (yes or no) answers do not meet the needs of the program. The explanation must be sufficiently clear that other reviewers, including non- medical staff, can see how the medical decision was reached. References from the medical literature may be used as part of the explanation.
4. In answering the claims examiner's questions, please be as definite as the medical findings in the case allow. Expressions such as "reasonable probability" and "likely" are acceptable to the program. In contrast, wording such as "might be due to" or "may have been caused" are too imprecise to support a claims decision.
If, while providing these services, problems or questions arise regarding a particular case or the program as a whole, please do not hesitate to call NAME on PHONE NUMBER. We will be glad to work with you to resolve any issues as they arise. When contacting us to discuss a problem related to a compensation case, please have the claim file number available.
Again, we appreciate your cooperation and look forward to your participation in our program.
Sincerely,
REGIONAL DIRECTOR
Back to Chapter 3-0900 Table of Contents
Exhibit 3: General Information for Physicians, Form CA-21 (Link to Image)
Back to Chapter 3-0900 Table of Contents
Exhibit 4: Sample Cover Letter—Case File Reviewer
Dear NAME OF PHYSICIAN:
Thank you for agreeing to perform case file reviews for the Federal Employees' Compensation Program.
Four copies of the Memorandum of Agreement are enclosed. Please sign three copies of the agreement form and return them together with your fee schedule to this office. We will then advise you when evaluations of case files are needed.
All medical opinions must contain detailed supporting rationale, based on actual findings and accepted medical opinion. Unsupported conjecture and speculative judgments cannot be accepted. Evaluations of percentage loss or loss of use of a member or function of the body for schedule award purposes must be made according to the AMA Guides, as far as possible. OWCP will provide further guidance for preparing medical reports as required.
No excerpts may be made from compensation files, and no case histories may be used for publication of any papers or books or in lectures without written permission of the Director, OWCP.
A provider under this agreement is an independent contractor and is not covered under the provisions of the Federal Employees' Compensation Act.
If you are currently providing a second opinion or referee evaluation to this office concerning any claimant, please so advise us, indicating the claimant's name and file number.
Again, we appreciate your cooperation and look forward to your participation in our program. If you have any questions, please contact NAME at TELEPHONE NUMBER.
Sincerely,
REGIONAL DIRECTOR
Enclosure: Memorandum of Agreement
Back to Chapter 3-0900 Table of Contents
Exhibit 5: Sample Memorandum of Agreement—Case File Reviewer
I. Introduction
This agreement provides for obtaining medical opinions required to determine entitlement to compensation under the Federal Employees' Compensation Act.
Case files reviews and evaluations of medical evidence are needed when the medical evidence of record is not clearly sufficient to support entitlement to benefits being claimed. In such circumstances, the case file is referred to a specialist in the appropriate field for an evaluation of the findings, diagnosis, and conclusions given the medical reports of record.
II. Services to be Provided
The physician shall review the medical reports and test results of record, the Statement of Accepted Facts prepared by OWCP, and any other pertinent information, and shall answer fully and with medical rationale each question posed by the OWCP. If the issue is degree of permanent impairment of a schedule member of the body, the physician shall include the date of maximum improvement and shall show how a percentage of impairment is derived in accordance (as far as possible) with the American Medical Association's Guides to the Evaluation of Permanent Impairment.
III. Reports
A full response to each question posed, with rationalized conclusions, shall be returned with the case file to the OWCP within 15 days after receipt by the reviewer.
IV. Method of Billing and Payment
Billings will be submitted on the form provided in each individual case, together with the physician's report. Fees will be paid in accordance with the negotiated fee schedule.
V. Fee Schedule
The basic fee for review of the file and narrative medical report is $00.
VI. Termination
This agreement may be canceled by either party upon thirty (30) days' written notice, and return of all OWCP materials.
VII. Security of Files
The physician or medical facility agrees that OWCP files and related material are to be treated in a confidential manner and made available only to individuals who need the files and other material to provide the services described in the agreement. OWCP files and related material will not be reproduced for any reason. When not in actual use, OWCP files and related material will be kept in secure storage under lock and key accessible only to those individuals who have a need for the files and related material for the purpose of providing services under this agreement. OWCP files and related material remain the property of the U.S. Department of Labor. This agreement confers no property rights in OWCP files and related material on the physician or medical facility providing service.
|
Contracting Officer |
Physician or Responsible Officer |
I am/am not currently providing treatment to beneficiaries of the Federal Employees' Compensation Act to the best of my knowledge. (If yes, provide a list of names.)
Physician's Employer Identification Number, or SSN, if not incorporated. (Show number under which payments should be reported to the Internal Revenue Service.)
State in which licensed:
State Board License Number: Expiration Date:
Back to Chapter 3-0900 Table of Contents

